Combining alcohol with prescription drugs isn’t just a bad idea-it can be deadly. Every year, thousands of people end up in emergency rooms or worse because they didn’t realize how dangerous mixing their meds with even one drink can be. This isn’t about binge drinking or partying. It’s about someone taking their blood pressure pill, having a glass of wine with dinner, and suddenly feeling dizzy, faint, or unable to breathe. These aren’t rare accidents. They’re predictable, preventable, and happening far more often than most people think.
How Alcohol Changes How Your Medicines Work
Alcohol doesn’t just sit there quietly in your body. It actively interferes with how your medications are processed. There are two main ways this happens: pharmacokinetic and pharmacodynamic interactions.
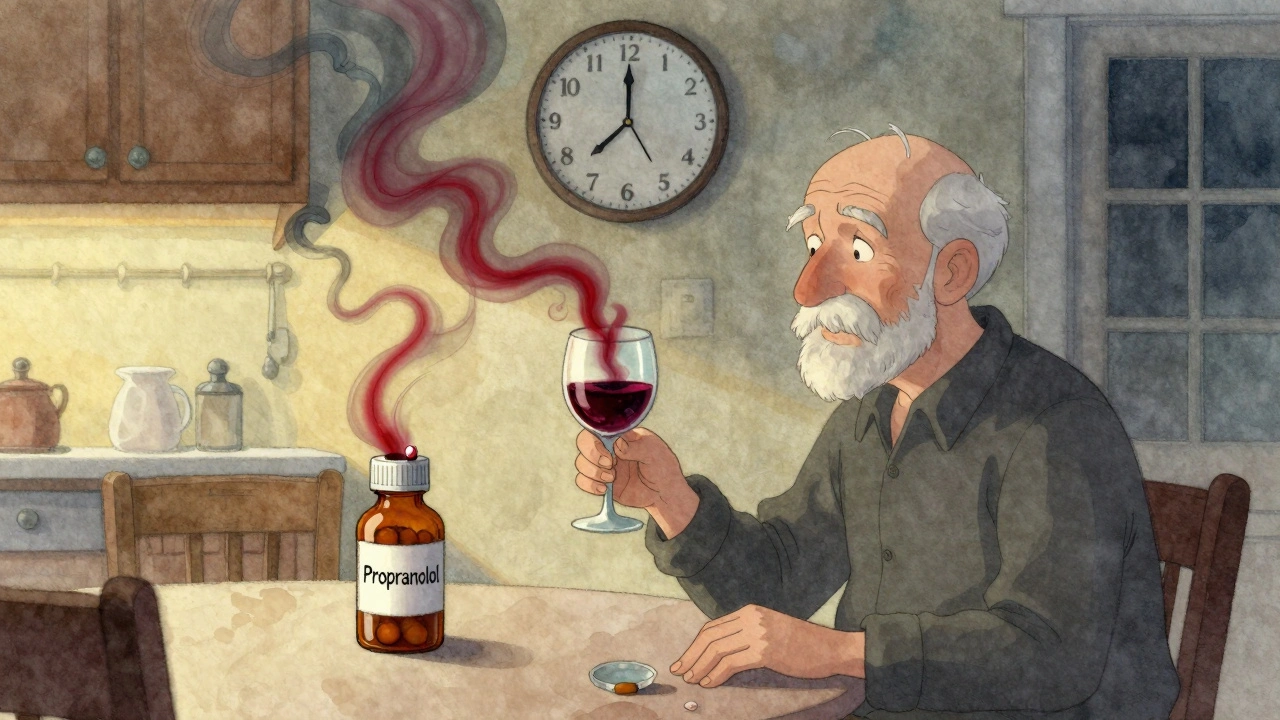
Pharmacokinetic interactions change how your body absorbs, breaks down, or gets rid of the drug. Most of this happens in your liver, where enzymes like CYP2E1 and CYP3A4 handle both alcohol and many common medications. When you drink regularly, your liver starts making more of these enzymes to deal with the alcohol. That means drugs like propranolol (a beta-blocker) get broken down faster-sometimes by 30% to 50%. The result? Your blood pressure stays high because the medicine isn’t working like it should.
On the flip side, having even one drink right before taking a pill can slow down those same enzymes. That’s dangerous with blood thinners like warfarin. Studies show alcohol can boost warfarin levels in your blood by up to 35%, increasing your risk of dangerous bleeding. You might not feel anything at first, but a minor bump could lead to internal bleeding you don’t notice until it’s too late.
Pharmacodynamic interactions are even scarier. This is when alcohol and the drug amplify each other’s effects on your body. Think of it like stacking two heavy weights on top of each other. Both alcohol and benzodiazepines like Xanax or Valium depress your central nervous system. Together, they don’t just add up-they multiply. Research shows this combo increases sedation by 400% compared to either one alone. That means extreme drowsiness, confusion, slow breathing, or even coma.
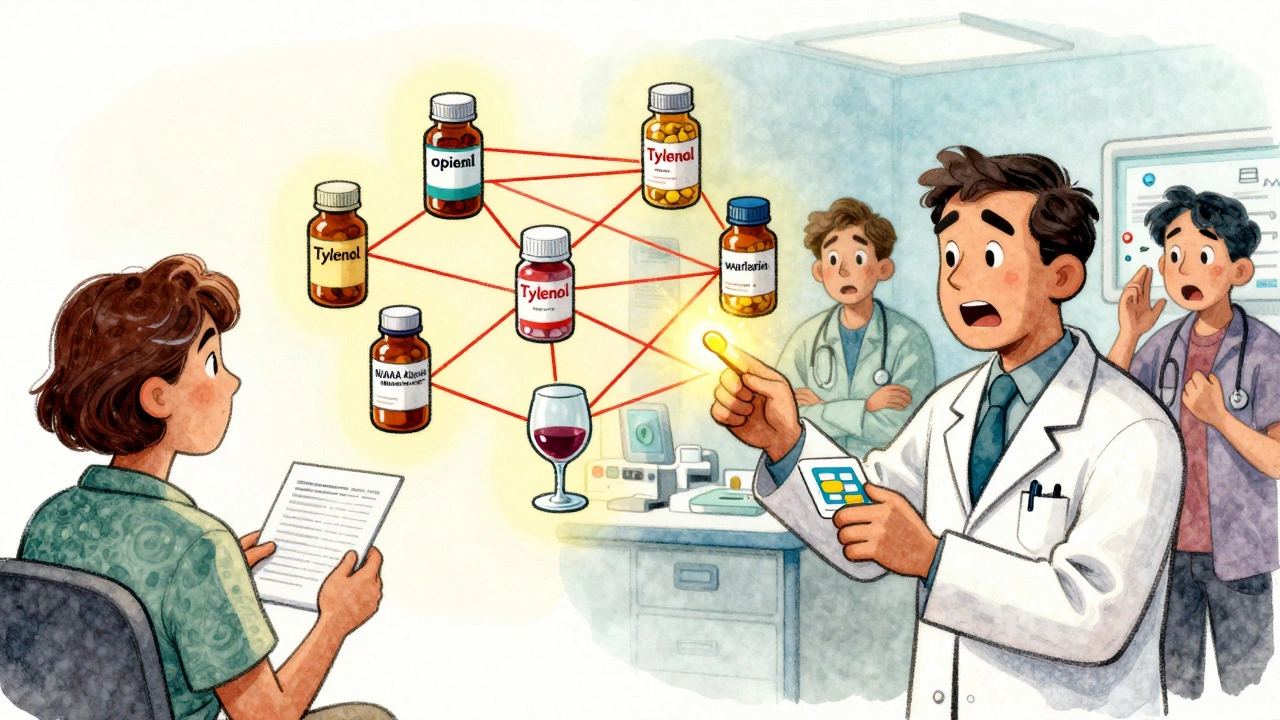
High-Risk Medications You Need to Avoid Alcohol With
Not all drugs are equally dangerous with alcohol. Some are okay in small amounts. Others? Never mix them. The highest-risk categories are clear:
- Opioids (oxycodone, hydrocodone, morphine): Alcohol + opioids multiplies the risk of fatal respiratory depression by six times. Even one drink with a prescribed painkiller can be enough to stop your breathing. In 2022, alcohol-opioid combinations were linked to 2,318 overdose deaths in the U.S. alone.
- Benzodiazepines (alprazolam, diazepam, lorazepam): These are prescribed for anxiety, insomnia, or seizures. With alcohol, they cause extreme dizziness, loss of coordination, and memory blackouts. In older adults, this combo increases fall risk by 50%. Many nursing home falls tied to sedatives happened within six hours of someone drinking.
- Acetaminophen (Tylenol): This common pain reliever is fine on its own-but with alcohol, it turns toxic. Your liver converts acetaminophen into a harmful byproduct. Alcohol pushes this process into overdrive. In regular drinkers, 1 in 200 people develop acute liver failure from this combo. It doesn’t take much: three drinks a week, plus daily Tylenol, can be enough.
- NSAIDs (ibuprofen, naproxen): These anti-inflammatories already irritate your stomach lining. Alcohol does the same. Together, they raise the risk of gastrointestinal bleeding by 300% in heavy drinkers. That’s not just an upset stomach-it’s internal bleeding that can require hospitalization.
- Antidepressants (SSRIs like sertraline, fluoxetine): While not usually deadly, alcohol makes side effects like drowsiness, dizziness, and impaired judgment much worse. One study found 35% of patients over 65 experienced dangerous drowsiness from just one or two drinks with their antidepressant.
Even some antibiotics can be risky. Isoniazid, used to treat tuberculosis, causes liver damage in 15% of people who drink while taking it. Other antibiotics like metronidazole trigger severe nausea, vomiting, and rapid heartbeat if mixed with alcohol.
Who’s Most at Risk?
It’s not just about what you’re taking-it’s about who you are.
People over 65 are at the highest risk. Their livers process alcohol and drugs slower. Their bodies have less water, so alcohol stays in their bloodstream longer. Studies show seniors experience 3.2 times more severe interactions than younger adults. And yet, 42% of U.S. adults over 65 regularly take medications that interact dangerously with alcohol.
Women are also more vulnerable. Even when they drink the same amount as men, women have higher blood alcohol levels because of differences in body composition. That means they’re more likely to experience stronger effects from the same drug-alcohol combo.
People with liver disease are in even greater danger. If your liver is already damaged from hepatitis, fatty liver, or years of drinking, adding alcohol to any medication can push it into failure. One study showed liver disease patients have a fivefold higher risk of acetaminophen toxicity when they drink.

Why So Many People Don’t Know the Risks
Here’s the scary part: most people aren’t warned.
Healthcare providers often don’t bring it up. A review of patient reviews on Healthgrades found 68% of people prescribed benzodiazepines were never told to avoid alcohol. One Reddit user shared how they were given oxycodone after surgery with no warning. Two beers later, they couldn’t breathe for 20 minutes. Another person said their pharmacist refused to fill their lorazepam prescription after learning they drank regularly-“probably saved my life.”
Even the labels on prescriptions are inconsistent. Only 38% of benzodiazepine prescriptions include a clear alcohol warning, according to an FDA audit. And most patients don’t read the fine print. A WebMD survey found 57% of adults wrongly believe one drink is safe with most medications. A third think only hard liquor is dangerous-when beer and wine are just as risky.
What You Should Do
Don’t wait for a warning. Take control.
- Check every prescription label. Look for words like “avoid alcohol,” “do not drink,” or “may cause drowsiness.” If it’s not there, assume it’s risky.
- Ask your pharmacist. Pharmacists are trained to spot these interactions. Bring a list of all your meds-including supplements and over-the-counter drugs. Use the four-question screening tool: Do you drink? How much? How often? And when was your last drink?
- Use a free tool. The NIAAA has a free app called “Alcohol Medication Check.” It lets you scan or search your meds and tells you if alcohol is dangerous with them. It covers over 2,300 medications.
- Be honest. If you drink-even just a glass of wine a few nights a week-tell your doctor. They can adjust your dose, switch your medication, or help you quit safely.
Some doctors argue that for low-risk meds, one drink a day might be okay. But the consensus from the American Medical Association, the American Pharmacists Association, and the American Geriatrics Society is clear: when in doubt, skip it. The risks aren’t worth it.
The Bigger Picture
This isn’t just an individual problem-it’s a systemic one. The global market for software that detects drug interactions is growing fast, hitting $2.84 billion by 2030. Hospitals are starting to use real-time systems that flag alcohol interactions before a prescription is filled. The VA has mandatory screening in 89% of its facilities. But private clinics? Only 32% do it.
Regulations are catching up. In 2022, the Alcohol-Drug Interaction Labeling Act required clear warnings on high-risk prescriptions. More states now require doctors to get training on substance-medication interactions to renew their licenses.
Still, the biggest barrier isn’t technology-it’s awareness. Only 28% of people at high risk actually stop drinking when warned. That’s why education has to start with you. If you’re on medication, don’t assume it’s safe. Don’t wait for a warning. Ask. Check. Protect yourself.
Can I have one drink with my prescription medication?
It depends on the medication. With opioids, benzodiazepines, or acetaminophen, even one drink can be dangerous. With some antibiotics or blood pressure pills, a single drink might not cause immediate harm-but it’s still risky. The safest answer is no. There’s no universal safe amount. Always check with your pharmacist or doctor before drinking.
What if I forgot and had a drink while on medication?
If you only had one drink and feel fine, monitor yourself for dizziness, drowsiness, nausea, or trouble breathing. Don’t take another dose of your medication until you’re sure you’re okay. If you feel unwell-especially if you’re on opioids or benzodiazepines-seek medical help immediately. Don’t wait. Call 911 or go to the ER.
Do over-the-counter meds like Tylenol interact with alcohol?
Yes. Acetaminophen (Tylenol) and alcohol together can cause serious liver damage-even if you’re not a heavy drinker. Taking just 2,000 mg of acetaminophen a day (four pills) while drinking three or more drinks a week increases your risk of liver failure. This isn’t just for alcoholics. It can happen to anyone who takes pain relievers regularly and has a drink now and then.
Is it safe to drink the day after taking a medication?
Not always. Some medications stay in your system for days. For example, metronidazole can cause reactions up to 72 hours after your last dose. Even if you feel fine, the drug may still be active. Always follow the label’s instructions. If it says “avoid alcohol during treatment and for X days after,” don’t ignore it.
Can alcohol make my medication less effective?
Yes. Chronic drinking can speed up how fast your body breaks down certain drugs, like beta-blockers or some antidepressants. That means your medication might not work as well. Your blood pressure could stay high, your anxiety might not improve, or your diabetes could become harder to control. You might think the drug isn’t working, when it’s actually the alcohol interfering.
Next Steps
If you’re on any prescription medication, take five minutes today to check your list. Look at the labels. Open the NIAAA app. Call your pharmacy and ask if your meds interact with alcohol. Don’t rely on memory. Don’t assume it’s fine because you’ve never had a problem before. The first time you mix alcohol with a dangerous drug might be the last.
And if you’re a caregiver for an older adult or someone with chronic illness, speak up. Many seniors won’t admit they drink. They think it’s harmless or don’t want to be judged. Gently ask. Help them check their meds. It could save their life.
Raja Herbal
December 7, 2025 AT 17:55So let me get this straight - we’ve got a whole essay on how alcohol + meds = death, but no one ever tells you this when they hand you the script? My uncle took oxycodone after knee surgery, had one beer, passed out on the toilet. They found him with his pants around his ankles and a half-eaten burrito on his lap. He’s fine now. But the doctor? Didn’t even blink. Just said, 'You should’ve read the label.' Bro, I didn’t even know labels came with instructions.
Evelyn Pastrana
December 8, 2025 AT 02:29Y’all act like this is news. My grandma takes blood pressure meds, drinks wine every night, and still dances at family weddings. She’s 82. Healthy as a horse. Maybe the real problem isn’t the alcohol - it’s that we treat older people like fragile glass figurines now. One drink isn’t a death sentence. It’s just a glass of wine. Chill out. Also, Tylenol + alcohol? Yeah, bad. But I’ve seen people die from eating too much peanut butter. We need better priorities.
Carina M
December 8, 2025 AT 09:53It is, without hyperbole, a moral failing of contemporary medical culture that such fundamental pharmacological knowledge remains uncommunicated to the lay populace. The absence of standardized, unambiguous warnings on prescription containers constitutes a dereliction of professional duty. One is left to wonder whether the commodification of healthcare has rendered the physician-patient relationship so transactional that even the most elementary safety protocols are deemed expendable. This is not merely negligence - it is epistemic negligence.
Maria Elisha
December 10, 2025 AT 05:34Ugh. Another one of these posts. I take Zoloft and have a glass of wine. I’m fine. If you’re gonna write a novel about every possible interaction, can we at least get a summary? Like a bullet point list? I don’t have time to read 2000 words before my 7pm cocktail.
Angela R. Cartes
December 10, 2025 AT 12:20So… like… I get it. Alcohol + meds = bad. 😬 But also… why are we still pretending that 'one drink' is a thing? If you're on benzodiazepines, you're already not in a good place mentally. Why are you drinking? Just… don't. Also, the NIAAA app? Cute. But if you're using it, you probably already know you're doing something dumb. 🤦♀️🍷
Andrea Beilstein
December 12, 2025 AT 05:59Alcohol isn't the enemy. The system is. We're told to take pills for everything then told not to enjoy life. We're given a diagnosis then handed a warning label like it's a punishment. What if the real interaction isn't between alcohol and medicine - but between human beings and a culture that treats healing like a compliance checklist? I've seen people die from loneliness. I've never seen anyone die from one glass of wine. But hey - maybe I'm just wrong. 🌿
om guru
December 13, 2025 AT 19:01Respectfully, the data presented is accurate and the risks are well documented. It is imperative that individuals under pharmacological treatment consult with licensed professionals before consuming ethanol. The liver is not a filter. It is a metabolic engine. Misuse leads to systemic failure. Prevention requires discipline. Education requires humility. Please do not gamble with your physiology.
Asset Finance Komrade
December 14, 2025 AT 23:12Interesting. But let’s interrogate the framing. Why is alcohol singled out? Coffee interacts with 90% of antidepressants. Caffeine + SSRIs = jittery anxiety spikes. Yet no one writes 3000-word essays about it. Why? Because wine is cultural. Coffee is capitalist. The moral panic around alcohol is less about science and more about Victorian guilt wrapped in a public health pamphlet. Also, 🍷