When you're managing Type 2 diabetes, taking multiple pills every day can be overwhelming. That’s why doctors often turn to diabetes combination medications-pills that pack two or more drugs into one tablet. These aren’t just convenient; they’re designed to work better together than alone. But here’s the catch: not all combination pills are created equal, especially when it comes to generics. If you’re switching from a brand-name combo to a generic, or thinking about it, you need to know what’s really going on inside that pill-and how it might affect your blood sugar.
What Are Diabetes Combination Medications?
Diabetes combination medications merge two different types of glucose-lowering drugs into a single tablet. Most of them include metformin-the first-line treatment for Type 2 diabetes-paired with another drug from a different class. The goal? Hit blood sugar from multiple angles at once. Metformin reduces liver glucose production and improves insulin sensitivity. Add a DPP-4 inhibitor like sitagliptin, and you boost insulin release after meals. Throw in an SGLT2 inhibitor like empagliflozin, and your kidneys start flushing out extra sugar through urine. These combos don’t just add up; they multiply effectiveness.Studies show these combinations typically lower HbA1c by 1.2% to 1.8%, compared to 0.7% to 1.0% with single drugs. That’s a big deal-because every 1% drop in HbA1c cuts your risk of diabetes complications by about 35%. And since many patients struggle to stick to multiple pills, combo meds improve adherence by up to 37%, according to a 2019 study in the Journal of Managed Care & Specialty Pharmacy.
Why Generic Versions Matter
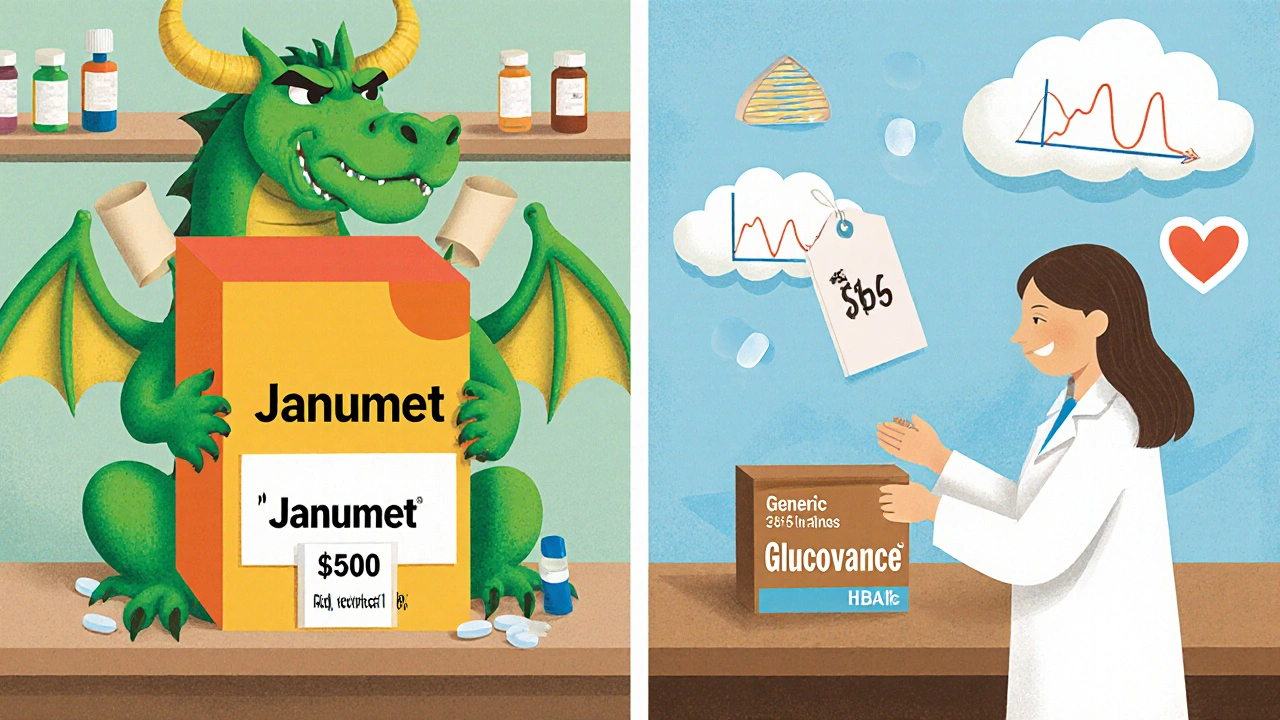
Brand-name combination drugs like Janumet (sitagliptin/metformin) or Synjardy (empagliflozin/metformin) can cost over $500 a month without insurance. That’s not sustainable for most people. Enter generics. They’re chemically identical to the brand versions, approved by the FDA, and often cost 85-95% less. For example, generic Metaglip (glipizide/metformin) runs about $18 for a 60-pill supply. Generic Glucovance (glyburide/metformin) is even cheaper at $15. That’s not a bargain-it’s a lifeline.But here’s the reality: only 5 out of the 25 combination diabetes meds on the U.S. market have generic versions. The rest? Still locked behind patents. If your doctor prescribed you a newer combo like Jardiance Met (empagliflozin/metformin), you’re stuck with the brand-until at least 2026. Patents protect these newer drugs, and manufacturers use legal tactics to delay generics. Meanwhile, older combos like those with sulfonylureas have been generic for over a decade.
Which Combination Meds Have Generic Versions?
Not all combos are equal when it comes to generics. Here’s what’s actually available right now:
- Metaglip (glipizide/metformin) - Generic since 2012. Available in 2.5/500mg and 5/500mg. Cash price: ~$18 for 60 tablets.
- Glucovance (glyburide/metformin) - Generic since 2010. Strengths: 1.25/250mg, 2.5/500mg, 5/500mg. Cash price: ~$15 for 60 tablets.
- Jentadueto (linagliptin/metformin) - First generic approved in May 2023, but not widely available until 2025 due to patent litigation.
- Janumet (sitagliptin/metformin) - Still brand-only. Generic expected around 2025-2026.
- Synjardy (empagliflozin/metformin) - No generic. Patent protection lasts until 2026.
Notice a pattern? The generics are almost all older combos with sulfonylureas. Newer classes like SGLT2 inhibitors and DPP-4 inhibitors are still under patent protection. That means if your doctor prescribes a newer combo, you’ll likely pay full price unless you qualify for a manufacturer’s patient assistance program.
Switching from Brand to Generic: What to Expect
Switching from a brand-name combo to its generic isn’t like swapping one brand of cereal for another. Diabetes meds have narrow therapeutic windows-small changes in blood concentration can lead to big changes in blood sugar. The FDA requires generics to be within 80-125% of the brand’s absorption rate. That sounds fine on paper. But for some patients, even a 10% difference in how fast or how much drug hits the bloodstream can trigger hypoglycemia or higher glucose spikes.
Real-world reports back this up. A 2022 survey by the American Pharmacists Association found that 12% of pharmacists had noticed patients experiencing unexpected side effects after switching to a generic combo. On Reddit’s r/Diabetes, 31% of users reported noticing changes in blood sugar patterns after switching to generic Glucovance or Metaglip. One user, 'Type2Warrior,' experienced recurrent low blood sugar after switching from brand Glucovance to generic-because the glyburide component released differently.
That’s why switching isn’t a one-time event. You need to monitor closely. The American Association of Clinical Endocrinology recommends checking your blood sugar 4 times a day for 2-4 weeks after switching. Keep a log. Note any unusual fatigue, dizziness, or spikes. If something feels off, don’t assume it’s just “adjusting.” Call your doctor.
Why Some People Can’t Switch
Not everyone can use a generic combo-even if it’s available. Here’s why:
- Extended-release (XR) formulations: Most generics are only available as immediate-release. If your doctor prescribed Janumet XR (extended-release sitagliptin/metformin), there’s no generic XR version yet. You can’t substitute an immediate-release generic for an XR brand-different release profiles mean different effects.
- Dose flexibility: Combination pills have fixed ratios. If you need 50mg sitagliptin and 1000mg metformin, Janumet XR 50/1000mg works. But if you need 100mg sitagliptin and 500mg metformin? No combo exists for that exact mix. With generics, you’re stuck with the available strengths. Sometimes, you’re forced to take two pills to match your dose-defeating the purpose of the combo.
- Renal function: Metformin is cleared by the kidneys. If your eGFR drops below 30, you can’t take any metformin combo-generic or brand. Some patients with borderline kidney function are switched to non-metformin combos, which rarely have generics at all.

Cost vs. Risk: Who Benefits Most from Generics?
Generics are a win for people on fixed incomes, those without good insurance, or those hitting Medicare’s coverage gap. For stable patients who’ve been on the same combo for years with consistent results, switching to a generic is often safe and smart. The Joslin Diabetes Center found that 76% of patients switched to generic Metaglip or Glucovance had no issues.
But for others, the risks outweigh the savings:
- Patients with unpredictable blood sugar swings
- Those with kidney issues or on other drugs that interact with metformin
- People who’ve had side effects from one component (e.g., nausea from metformin, low blood sugar from sulfonylureas)
- Those who need precise titration of one drug without changing the other
In these cases, staying on brand may be the safer, more effective choice-even if it costs more. Insurance sometimes requires prior authorization for brand-name combos, but your doctor can appeal with documentation of medical necessity.
What You Can Do Right Now
If you’re on a diabetes combo and worried about cost or switching:
- Ask your pharmacist: Is your current combo available as a generic? What’s the exact name and strength?
- Check your insurance: Does your plan require generic substitution? Can you get a prior authorization for the brand if needed?
- Use GoodRx or RxSaver: Compare cash prices. Sometimes the brand is cheaper with a coupon than the generic without one.
- Ask about patient assistance: Merck, Boehringer Ingelheim, and others offer free or low-cost programs for brand-name combos if you qualify.
- Track your blood sugar: If you switch, test more often for the first month. Don’t assume it’s the same.
- Don’t self-switch: Never change your meds without talking to your doctor. Pharmacy substitution without medical approval is risky and has led to treatment failures in 19% of endocrinologists’ patients, per the American Association of Clinical Endocrinology.
The Future of Generic Diabetes Combos
The tide is turning. Patents on Janumet XR and other DPP-4/metformin combos expire in 2024-2026. By 2027, experts predict over half of all combination prescriptions will be generic. Evaluate Pharma forecasts that generic entry could save the U.S. healthcare system $2.1 billion annually. The Congressional Budget Office estimates average annual costs for combination therapy could drop from $2,850 to $420 per patient.
But this doesn’t mean everyone will automatically save. Generic manufacturers often only produce the most common strengths and immediate-release forms. If you need something specific, you might still need the brand. And until all combos are generic, the gap between what’s affordable and what’s medically ideal will remain.
The bottom line? Generics are powerful tools-but they’re not magic. They work best when you understand them, monitor their effects, and work with your care team-not just your pharmacy.
Can I switch from a brand-name diabetes combo to a generic without talking to my doctor?
No. Even though pharmacies can legally substitute generics in some cases, diabetes combination medications are not like antibiotics or blood pressure pills where substitution is low-risk. Small changes in drug absorption can cause dangerous blood sugar swings. The American Association of Clinical Endocrinology warns that 19% of endocrinologists have seen treatment failures after automatic pharmacy substitutions. Always consult your doctor before switching.
Why are some diabetes combo generics so cheap while others are still expensive?
It’s all about patents. Older combos like Metaglip (glipizide/metformin) and Glucovance (glyburide/metformin) use drugs whose patents expired over a decade ago. Generic manufacturers can produce them for pennies. Newer combos like Synjardy (empagliflozin/metformin) or Janumet (sitagliptin/metformin) are protected by patents that last 20+ years. Manufacturers also file additional patents on formulations or delivery methods to delay generics. Until those expire, you’ll pay full price.
Are generic diabetes combos as effective as brand-name ones?
For most people, yes-when used correctly. The FDA requires generics to meet strict bioequivalence standards. But bioequivalence doesn’t mean identical in every patient. Some people are more sensitive to small differences in how the drug is absorbed. Studies show 80-90% of patients experience no change in effectiveness after switching. But 10-20% notice changes in blood sugar control or side effects. That’s why monitoring is critical after switching.
Can I take a generic metformin with a separate generic of another drug instead of a combo pill?
Yes, and sometimes it’s smarter. If you’re on a combo that doesn’t have a generic version, you can often take the two separate generic drugs instead. For example, if Janumet is too expensive, you could take generic metformin and generic sitagliptin (if available) separately. This gives you more flexibility to adjust doses. But you’ll be taking two pills instead of one, and it may cost more overall. Talk to your doctor or pharmacist to compare total cost and convenience.
Do generic diabetes combos have different side effects?
The active ingredients are the same, so side effects should be similar. But inactive ingredients-like fillers, dyes, or coating materials-can differ. Some patients report more stomach upset, nausea, or changes in pill size after switching. A 2022 GoodRx review found 22% of users reported new gastrointestinal issues after switching to generic Glucovance. If side effects start after a switch, it’s worth discussing with your doctor. It might not be the drug-it might be the filler.
What should I do if my insurance forces me to switch to a generic I don’t want?
Ask your doctor to file a prior authorization appeal. Explain why the brand is medically necessary-for example, if you’ve had side effects with generics, need an extended-release form, or have unstable blood sugar. Many insurers approve appeals with proper documentation. You can also check if the manufacturer offers a copay card. For example, Merck’s Janumet patient assistance program can reduce costs to $0 for eligible patients.

Steve Phillips
November 10, 2025 AT 23:05Oh, for crying out loud-another ‘generic is fine’ lecture? You’re telling me I can just swap my Janumet for some lab-rat concoction and expect my HbA1c to behave? The FDA’s 80–125% bioequivalence window? That’s not science-it’s a casino! I’ve seen people crash into hypoglycemia because some generic’s glyburide dissolved like a sugar cube in tea instead of a slow-burn candle. And don’t get me started on the fillers-some of these generics have more talc than my ex’s excuses.
And yes, I know it’s cheaper-but when your kidneys are whispering ‘please stop’ and your glucose monitor is screaming ‘DANGER’, cheap doesn’t save lives-it just saves corporate profits.
Erika Puhan
November 12, 2025 AT 04:44Let’s deconstruct this. The article presents a false dichotomy between ‘brand = safe’ and ‘generic = risky.’ But bioequivalence is statistically validated across population-level pharmacokinetics. The 10–20% who report variability? That’s within the expected inter-individual variability of any drug class-especially those with narrow therapeutic indices. The real issue isn’t the generic-it’s the lack of individualized therapeutic monitoring protocols.
Moreover, the reliance on Reddit anecdotal data as evidence is methodologically unsound. The sample is self-selected, non-randomized, and confounded by confirmation bias. Until we see RCTs with CGM-derived AUC data, this is just fearmongering dressed as patient advocacy.
Kelsey Veg
November 12, 2025 AT 10:56ok so i switched to generic glucovance last month and my sugar has been all over the place. like, 5am lows and 2pm highs. i thought it was just stress or coffee or something but then i checked the pill-same name, different color, different shape. now i’m scared to even take it. my pharmacist said ‘it’s the same thing’ but… it’s not. my body knows.
Alex Harrison
November 14, 2025 AT 03:33I’ve been on metformin + sitagliptin for five years. When the generic for Jentadueto finally hit, my insurance pushed me to switch. I monitored like crazy-four times a day for six weeks. No changes. My HbA1c stayed at 6.8. I saved $420/month. I’m not a lab rat-I’m just a guy who doesn’t want to choose between meds and groceries.
Yes, some people have issues. But assuming everyone will? That’s like saying all cars with the same engine are unsafe because one guy had a bad transmission.
Jay Wallace
November 15, 2025 AT 12:38So now we’re letting Chinese and Indian labs make our life-saving meds? That’s just asking for disaster. The FDA doesn’t inspect those plants like they do here. You think they care about your glucose levels? They care about profit margins. And now you want me to trust some pill that costs $15 because ‘it’s the same chemicals’? Newsflash: chemistry isn’t everything. Manufacturing matters. Quality control matters. And right now, we’re outsourcing our health to countries that don’t even have the same legal standards.
Alyssa Fisher
November 16, 2025 AT 10:20There’s something deeply human about this whole debate. We treat our medications like sacred objects-each pill a promise, each dose a ritual. When the shape changes, the color shifts, the imprint fades-it’s not just chemistry that’s altered. It’s trust. And for someone whose body already feels like a battlefield, that’s a lot to lose.
But here’s the quiet truth: the system isn’t broken because generics exist. It’s broken because we force people to choose between dignity and survival. Maybe the real question isn’t ‘are generics safe?’ but ‘why do we let cost dictate access to stability?’
Alyssa Salazar
November 18, 2025 AT 07:10Okay, but let’s be real-how many people even know what’s in their combo pills? I had a patient last week who thought ‘metformin’ was a brand name. She was taking two different generics because she thought they were different drugs. The system is so fragmented that even if generics were perfect, the education gap makes this a minefield.
And the fact that XR versions don’t have generics? That’s criminal. If you need extended release, you’re stuck paying $500/month. That’s not healthcare-it’s extortion. Pharma’s playing chess while patients are playing Jenga.
Beth Banham
November 19, 2025 AT 03:34I switched to generic Glucovance last year. No issues. My sugar’s steady. I sleep better now because I’m not stressing about the bill. I get that it doesn’t work for everyone-but for me? It was a gift. I’m not trying to convince anyone to switch. Just saying… it’s okay if it works for you too.
Brierly Davis
November 20, 2025 AT 01:40Biggest tip I can give: if you switch, test like your life depends on it-because it kinda does. I did 8 tests a day for the first 10 days after switching. Took notes. Showed my doctor. He adjusted my dose by 10% and now I’m golden. You don’t have to suffer through it. You just have to be proactive.
And hey-if you’re worried, ask about patient assistance. Merck’s program got my Janumet down to $0. No shame in asking for help. We’re all just trying to survive this.
Amber O'Sullivan
November 20, 2025 AT 22:22