For many seniors with diabetes, the biggest danger isn’t high blood sugar-it’s low blood sugar. A single episode of hypoglycemia can lead to a fall, a hospital visit, or even death. And yet, too many older adults are still prescribed medications that put them at high risk. The truth is, not all diabetes drugs are created equal when it comes to safety in seniors. Some can be deadly. Others are safe, effective, and life-changing. The key isn’t just controlling blood sugar-it’s avoiding low blood sugar altogether.
Why Hypoglycemia Is So Dangerous for Seniors
Low blood sugar, or hypoglycemia, means glucose levels drop below 70 mg/dL. For a young, healthy person, this might mean a quick snack and a quick recovery. For an 80-year-old with weak muscles, poor balance, or heart disease, it’s a medical emergency. When blood sugar drops, the brain doesn’t get enough fuel. That leads to dizziness, confusion, sweating, shaking, or sudden fatigue. These symptoms don’t just feel bad-they cause falls. And falls in seniors often mean broken hips, head injuries, or long-term disability.Research shows that one severe hypoglycemic episode in someone over 65 increases the chance of dying within a year by 60%. That’s not a small risk. It’s a life-or-death one. Even mild lows-between 54 and 69 mg/dL-can trigger heart rhythm problems or strokes in older adults. The body’s natural defenses against low blood sugar also weaken with age. Hormones like glucagon and epinephrine, which normally kick in to raise blood sugar, don’t respond as quickly or strongly. That means seniors don’t feel the warning signs until it’s too late.
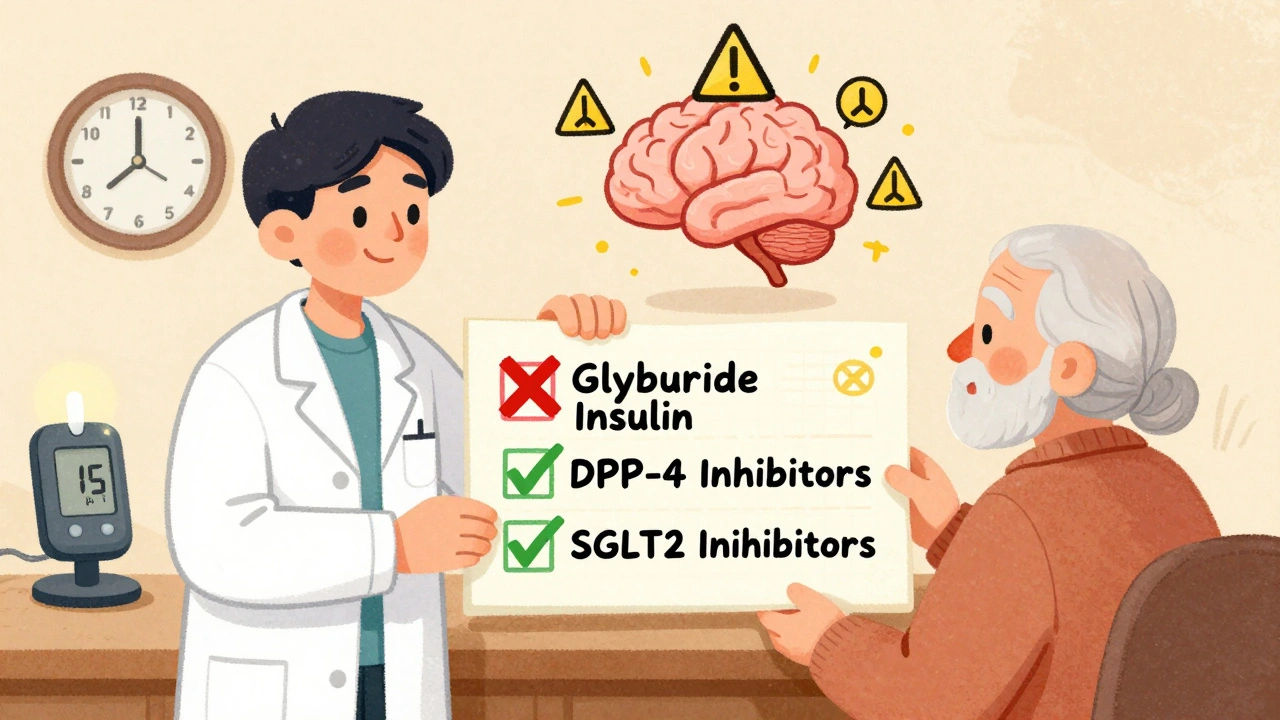
Medications That Put Seniors at Highest Risk
Not all diabetes pills or insulin shots are risky-but some are far more dangerous than others. The biggest culprit? Glyburide, a sulfonylurea sold under brand names like Glynase and Micronase. This drug forces the pancreas to pump out insulin all day, no matter what. In younger people, that works fine. In seniors, it’s a recipe for trouble.Glyburide stays in the body for too long, especially if kidney function is reduced-which is common after 65. Studies show that nearly 40% of elderly patients on glyburide have at least one hypoglycemic episode per year. That’s more than double the rate seen with other sulfonylureas like glipizide. Because of this, the American Geriatrics Society lists glyburide as a medication seniors should avoid entirely. The FDA now requires warning labels on all sulfonylureas stating they increase hypoglycemia risk in older adults with kidney issues.
Insulin is another major risk. While it’s powerful and effective, it requires precise timing and matching food intake. Many seniors forget meals, eat inconsistently, or can’t manage multiple daily injections. A 2010 study found insulin use increases fall risk by 30% in older adults due to dizziness from low blood sugar. Even long-acting insulin like glargine can cause dangerous nighttime lows that go unnoticed until morning.
The Safest Diabetes Medications for Seniors
The good news? There are safer options. Newer drugs don’t force the body to make more insulin. They work differently-and they’re much gentler.DPP-4 inhibitors like sitagliptin (Januvia), linagliptin (Tradjenta), and saxagliptin (Onglyza) are among the safest. These drugs help the body use its own insulin more efficiently, but only when blood sugar is high. They don’t cause lows on their own. Clinical trials show hypoglycemia rates with these drugs are only 2-5% when used alone-compared to 30-40% with glyburide. Many seniors on DPP-4 inhibitors report feeling more stable, with fewer episodes of shakiness or confusion.
SGLT2 inhibitors like empagliflozin (Jardiance) and dapagliflozin (Farxiga) work by helping the kidneys flush out extra sugar through urine. They rarely cause hypoglycemia unless combined with insulin or sulfonylureas. Studies show their hypoglycemia rate is around 4.5%, similar to placebo. Plus, they offer extra benefits: lower blood pressure, reduced heart failure risk, and slower kidney decline-all common concerns in older adults.
Metformin is still considered a first-line option for many seniors, but only if kidney function is normal. It doesn’t cause hypoglycemia on its own. But if creatinine clearance drops below 30 mL/min (common in those over 80), doctors should stop it. Too much metformin in someone with poor kidneys can lead to lactic acidosis, a rare but serious condition.
And then there’s tirzepatide (Mounjaro), a newer injectable approved in 2022. In trials with seniors, it caused hypoglycemia in only 1.8% of users-far lower than insulin. While it’s more expensive and requires weekly shots, it’s becoming a top choice for those who need stronger control without the danger of lows.

How to Spot Hypoglycemia Before It’s Too Late
Seniors often don’t feel the usual warning signs. Sweating, shaking, and a racing heart? Those may not happen. Instead, they might just feel tired, confused, or unusually irritable. Sometimes, they’ll say they’re “just not themselves.”Here’s what to watch for:
- Sudden dizziness or unsteadiness
- Confusion or trouble speaking
- Headache or nausea
- Weakness or feeling like you’re going to pass out
- Changes in behavior-like being unusually quiet, aggressive, or forgetful
- Nightmares or waking up drenched in sweat
Family members and caregivers need to learn these signs. If a senior seems “off,” check their blood sugar-even if they say they’re fine. A simple fingerstick test can prevent a hospital trip.
Monitoring and Technology That Saves Lives
Traditional fingerstick testing works, but it’s not enough. Seniors often forget to test, or don’t know when to test. Continuous glucose monitors (CGMs) change that. These small devices, worn on the arm or belly, track blood sugar 24/7 and send alerts when levels drop too low.A 2021 study found seniors using CGMs had 65% fewer hypoglycemic episodes than those relying on fingersticks. The alarms wake them up at night. They alert caregivers if someone is slumping in a chair. Some CGMs even sync with smartwatches or home monitoring systems. For seniors living alone, this isn’t just convenient-it’s life-saving.
Even basic glucose meters with memory and large displays help. Look for models that store readings, show trends, and let caregivers view data remotely. Many Medicare plans now cover CGMs for seniors with a history of hypoglycemia.
Medication Reviews and Avoiding Dangerous Mixes
Seniors with diabetes often take 5 or more medications. That’s called polypharmacy. And when you mix diabetes drugs with other pills, things can go wrong.For example:
- Beta-blockers (used for high blood pressure or heart issues) can hide the signs of low blood sugar, like a fast heartbeat. You won’t feel your heart racing-and that’s one of your body’s main warnings.
- NSAIDs like ibuprofen or naproxen can make sulfonylureas stronger, increasing hypoglycemia risk.
- Some antibiotics and antifungal drugs can also interfere with how diabetes medications work.
That’s why a full medication review every 3-6 months is critical. Pharmacists can spot dangerous combinations. The STOPP/START criteria-a tool used by geriatric specialists-helps identify which drugs should be stopped and which should be added. One study showed using this approach reduced hypoglycemia hospitalizations by 32%.
Don’t assume your doctor knows every pill you’re taking. Bring a list-physical or digital-to every appointment. Include vitamins, supplements, and over-the-counter meds. Even aspirin can interact.
What Seniors and Families Can Do Right Now
If you or a loved one has diabetes and is over 65, here’s what to do:- Ask your doctor: “Am I on a drug that could cause low blood sugar?” If you’re on glyburide, ask why-and if there’s a safer alternative.
- Request a CGM if you’ve had even one episode of hypoglycemia. Medicare covers it for those with a history of lows.
- Keep fast-acting sugar on hand: glucose tablets, juice boxes, or hard candy. Don’t wait for symptoms to get bad.
- Teach family members how to recognize and treat low blood sugar. Put a note on the fridge: “If they seem confused, check their sugar.”
- Ask for a pharmacist-led medication review. Many pharmacies offer this for free.
One 78-year-old woman, Mary Thompson, shared her story on the American Diabetes Association forum: “After my third fall from low blood sugar on glyburide, my doctor switched me to sitagliptin. In six months, I’ve had zero hypoglycemia episodes and feel much safer walking around my home.” That’s not luck. That’s better medicine.
Final Thought: Safety Over Numbers
Doctors used to push for HbA1c levels under 7% for everyone. That’s outdated. For seniors, the goal isn’t perfection-it’s safety. The American Diabetes Association now says: “Avoiding hypoglycemia is a higher priority than achieving near-normal glycemia.”That means an HbA1c of 7.5% to 8.5% might be perfect for an 82-year-old with heart disease and memory issues. Trying to force it lower could cost them their independence-or their life. The best diabetes care for seniors isn’t about hitting targets. It’s about staying out of the hospital, staying on their feet, and staying alive.

Isabelle Bujold
December 4, 2025 AT 16:17It's staggering how many elderly patients are still on glyburide-especially when we have safer, smarter options now. I've seen it firsthand in my geriatric practice: a 79-year-old man on glyburide fell three times in six months, all from unnoticed hypoglycemia. Switched him to linagliptin, and within weeks, his balance improved, his wife said he stopped zoning out at dinner, and his HbA1c stayed stable. The real tragedy isn't the drug-it's the inertia in prescribing. We're still treating diabetes like it's 1998. The guidelines changed. The evidence is clear. Why are we still risking lives for outdated protocols?
Yasmine Hajar
December 5, 2025 AT 16:13This is why I started teaching my mom’s senior group how to use CGMs. She was on metformin and insulin, and I didn’t even know she was having lows until she started calling me at 3 a.m. crying because she felt ‘like a ghost.’ We got her a FreeStyle Libre, and now she gets alerts on her phone and I get them too. Last week, she had a 58 mg/dL drop while watching TV-alarm went off, she ate a glucose tab, and kept watching ‘Judge Judy.’ No fall. No ER. No trauma. Technology isn’t magic-it’s mercy.
Jake Deeds
December 6, 2025 AT 13:35Let’s be honest-most doctors don’t even know what DPP-4 inhibitors are. They just keep prescribing the same pills they learned in med school 30 years ago. And don’t get me started on how Medicare makes it harder to get CGMs than a prescription for opioids. This isn’t healthcare-it’s bureaucratic negligence dressed in white coats. If your grandma’s glucose monitor still requires a finger prick, you’re not managing diabetes-you’re playing Russian roulette with her life.
Jenny Rogers
December 6, 2025 AT 21:54It is, of course, axiomatic that the medical-industrial complex prioritizes profit over patient welfare, and the continued prescription of sulfonylureas to the elderly is merely one of countless manifestations of this systemic moral failure. One must question not only the pharmacological rationale, but the epistemological foundations of contemporary geriatric care: are we treating disease, or merely commodifying biological processes? The fact that a drug like glyburide-known since the 1950s to have a half-life incompatible with renal senescence-remains in widespread use speaks volumes about the decay of evidence-based ethics in clinical practice.
George Graham
December 7, 2025 AT 00:05I’m a caregiver for my 84-year-old uncle who’s been on Januvia for a year now. He used to get dizzy after lunch and blame it on ‘getting old.’ Turned out his sugar was dipping to 52. We didn’t even know he was on glyburide until his new PCP found it in his med list. Switched him over, and now he’s walking to the corner store again. He even started gardening. It’s not about fancy tech-it’s about listening. And sometimes, just asking, ‘Have you felt weird lately?’ changes everything.
Carolyn Ford
December 7, 2025 AT 04:31Rachel Bonaparte
December 8, 2025 AT 11:07Did you know the FDA didn’t require those warning labels on sulfonylureas until 2021? That’s 50 years of elderly people dropping like flies and nobody doing anything. And now they want us to believe this is ‘better medicine’? Wake up. The same companies that made glyburide are now selling Jardiance and Mounjaro. It’s the same playbook: create a crisis, then sell the ‘solution.’ CGMs? Sure, they’re great-but they’re $300/month. Medicare won’t cover them unless you’ve had three ER visits. That’s not care. That’s extortion.
John Filby
December 9, 2025 AT 10:24