Diuretic Selection Guide
Clinical Scenario Selection
Key Decision Criteria
Recommended Diuretic
Select criteria and click "Generate Recommendation" to see results
Diuretic Comparison
Furosemide
Loop Diuretic
Bumetanide
Loop Diuretic
Torsemide
Loop Diuretic
Hydrochlorothiazide
Thiazide Diuretic
Spironolactone
Aldosterone Antagonist
Key Takeaways
- Furosemide is the most potent loop diuretic, ideal for rapid fluid removal.
- Hydrochlorothiazide works slower but is cheaper and often used for mild hypertension.
- Bumetanide and torsemide offer similar potency to furosemide with longer half‑lives.
- Spironolactone acts on a different pathway (aldosterone antagonism) and is useful when potassium‑sparing is needed.
- Choosing the right agent depends on onset speed, duration, kidney function, and side‑effect profile.
What Is Furosemide?
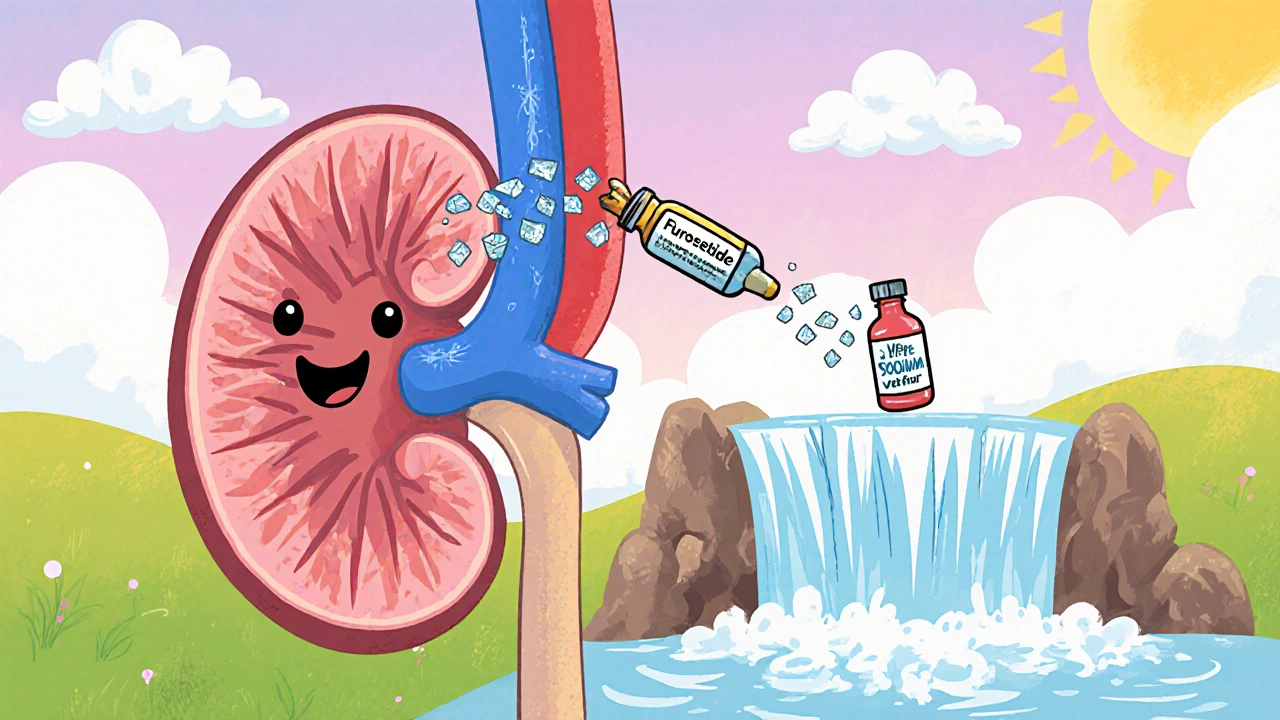
When it comes to diuretics, Furosemide is the go‑to choice for many clinicians. It belongs to the loop diuretic class and works by blocking the Na⁺‑K⁺‑2Cl⁻ transporter in the thick ascending limb of the nephron. This interruption forces the kidneys to excrete large volumes of sodium and water, quickly reducing fluid overload.
How Furosemide Works: Mechanism of Action
The transporter inhibition leads to three key effects:
- Heavy natriuresis (sodium loss) that drags water out of the bloodstream.
- Reduced reabsorption of calcium, which can be helpful in certain kidney stones.
- Activation of the renin‑angiotensin system, which explains why potassium‑sparing agents are sometimes added.
Because the loop is upstream of most other nephron segments, the diuretic effect is both rapid and profound.
Typical Clinical Uses of Furosemide
Doctors prescribe furosemide for conditions that demand fast fluid removal:
- Congestive heart failure (CHF) with pulmonary edema.
- Acute kidney injury where fluid overload threatens renal perfusion.
- Liver cirrhosis with ascites.
- Severe hypertension unresponsive to other agents.
Doses range from 20 mg orally to 40 mg IV, adjusted for renal function and response.
Alternative Diuretics: An Overview
The most common alternatives fall into three families: other loop diuretics, thiazide‑type diuretics, and aldosterone antagonists.
Bumetanide
Bumetanide is a loop diuretic that is roughly 40 % more potent than furosemide on a milligram‑for‑milligram basis. It has a shorter half‑life (about 1 hour) and is often used when rapid, high‑intensity diuresis is needed but with less volume overload.
Torsemide
Torsemide offers a longer duration of action (up to 12 hours) and a more predictable oral bioavailability (about 80 %). Its anti‑aldosterone properties give it a slight edge in heart‑failure patients who need both diuresis and neuro‑hormonal blockade.
Hydrochlorothiazide
Hydrochlorothiazide belongs to the thiazide diuretic class. It works farther downstream, blocking the Na⁺‑Cl⁻ transporter in the distal convoluted tubule. The result is a milder diuresis, making it suitable for chronic hypertension and mild edema.
Spironolactone
Spironolactone is an aldosterone antagonist. It prevents sodium reabsorption in the collecting duct while sparing potassium. Clinicians add it when patients on furosemide develop hypokalemia or when the goal is to blunt aldosterone‑driven fibrosis.
Decision Criteria: How to Pick the Right Diuretic
When comparing furosemide to its alternatives, keep these factors in mind:
- Onset Speed: Loop diuretics (furosemide, bumetanide, torsemide) act within minutes when given IV, while thiazides take hours.
- Duration of Effect: Torsemide lasts the longest; furosemide’s effect tapers after 6 hours.
- Potency: Bumetanide > furosemide > torsemide (per mg), thiazides are far less potent.
- Kidney Function: All loops require some renal clearance; thiazides lose efficacy when eGFR < 30 mL/min.
- Electrolyte Impact: Loops cause hypokalemia, thiazides lead to hyponatremia, spironolactone may cause hyperkalemia.
- Cost & Availability: Hydrochlorothiazide is the cheapest; torsemide and bumetanide are pricier but may reduce hospital stay length.
- Specific Indications: For acute pulmonary edema, furosemide or bumetanide is preferred; for long‑term hypertension, hydrochlorothiazide shines.
Side‑Effect Profile at a Glance
| Drug | Class | Onset (IV) | Duration (Oral) | Potency (mg) | Main Uses | Typical Side Effects |
|---|---|---|---|---|---|---|
| Furosemide | Loop | 5‑10 min | 6‑8 h | 1 mg ≈ 1 unit | CHF, AKI, ascites | Hypokalemia, ototoxicity, dehydration |
| Bumetanide | Loop | 5‑10 min | 4‑6 h | 0.5 mg ≈ 1 unit | Rapid diuresis, resistant edema | Hypokalemia, ototoxicity (less common) |
| Torsemide | Loop | 10‑15 min | 12‑14 h | 1 mg ≈ 1 unit | CHF with chronic management | Hypokalemia, mild GI upset |
| Hydrochlorothiazide | Thiazide | 30‑60 min | 12‑24 h | 25 mg ≈ 1 unit | Hypertension, mild edema | Hyponatremia, hyperuricemia, photosensitivity |
| Spironolactone | Aldosterone antagonist | 45‑60 min | 24‑48 h | 25 mg ≈ 1 unit | Hyperaldosteronism, potassium‑sparing in CHF | Hyperkalemia, gynecomastia, menstrual irregularities |
Choosing the Right Agent for Specific Scenarios
Acute pulmonary edema: furosemide or bumetanide gives the fastest relief. If the patient has a history of ototoxicity, torsemide may be safer.
Chronic heart‑failure maintenance: torsemide’s longer half‑life reduces dosing frequency, and its mild anti‑aldosterone effect adds benefit.
Hypertension with mild fluid retention: hydrochlorothiazide is cost‑effective and works well when kidney function is preserved.
Patients prone to low potassium: adding spironolactone can counteract loop‑induced hypokalemia, but monitor serum potassium closely.
Practical Tips and Pitfalls to Avoid
- Always check eGFR before starting a loop; doses may need reduction when eGFR < 30 mL/min.
- Monitor electrolytes daily for the first 72 hours of high‑dose furosemide therapy.
- If ototoxicity is a concern (e.g., high‑dose, prolonged IV use), consider switching to torsemide or using the lowest effective dose.
- Combine a loop with a potassium‑sparring agent (spironolactone or amiloride) only after confirming normal renal function.
- Educate patients to report sudden hearing loss, muscle cramps, or excessive thirst.
Frequently Asked Questions
Can I switch from furosemide to hydrochlorothiazide for chronic hypertension?
Yes, if the patient only needs mild diuresis and blood‑pressure control, hydrochlorothiazide offers a safer, once‑daily regimen. However, assess kidney function first; thiazides lose effect when eGFR drops below 30 mL/min.
Why does furosemide sometimes cause hearing loss?
High‑dose IV furosemide can damage the cochlea’s hair cells, especially in patients with pre‑existing kidney failure. Reducing the infusion rate or switching to torsemide can lower this risk.
Is bumetanide more effective than furosemide?
Bumetanide is about 40 % more potent per milligram, so lower doses achieve the same diuretic effect. It’s useful when fluid overload is severe but total fluid volume to be given is limited.
When should spironolactone be added to a loop diuretic?
Add spironolactone if the patient develops hypokalemia or has evidence of aldosterone‑mediated fibrosis (e.g., worsening heart failure despite optimal loop dosing). Start low and monitor potassium and creatinine.
Which diuretic is best for patients on dialysis?
Loop diuretics are generally ineffective in anuric dialysis patients because there’s no urine output to act upon. Instead, focus on ultrafiltration settings during dialysis. If residual urine remains, low‑dose furosemide may still help manage volume.
Next Steps for Clinicians and Patients
Start by assessing the clinical picture: acute vs chronic, kidney function, and electrolyte status. Choose the diuretic that matches the required onset and duration, then tailor the dose. Follow up with labs within 48 hours and adjust based on response. For patients, education about signs of dehydration, electrolyte imbalance, and hearing changes is crucial for safe use.
Latasha Becker
October 19, 2025 AT 21:23The pharmacokinetic profile of furosemide warrants a nuanced appreciation of its bioavailability, which hovers near 50 % orally due to extensive first‑pass metabolism, thereby necessitating dose titration predicated on renal clearance parameters.
Its loop‑mediated inhibition of the Na⁺‑K⁺‑2Cl⁻ cotransporter precipitates a marked natriuretic surge, compelling clinicians to monitor serum electrolytes with a frequency commensurate to dosage escalation.
In patients with eGFR below 30 mL/min, the fractional excretion advantage diminishes, prompting consideration of torsemide or bumetanide as pharmacodynamic alternatives.
Moreover, the ototoxic potential of high‑dose intravenous furosemide is mechanistically linked to cochlear hair‑cell stress, a fact that should inform risk‑benefit analyses in vulnerable cohorts.
Finally, integration of a potassium‑sparing agent such as spironolactone can mitigate hypokalemia, yet mandates vigilant surveillance of serum potassium and creatinine.
parth gajjar
October 20, 2025 AT 05:43It feels like the heart is about to burst when the fluid piles up and you watch that chest X‑ray swell like a balloon. The drama of a rapid IV push of furosemide is nothing short of cinematic. Yet the after‑effects whisper in the ears of the patient-cramps, dehydration, a faint ringing in the ears. This cascade makes every dose feel like a gamble.
Maridel Frey
October 20, 2025 AT 14:03For clinicians seeking a balanced approach, it is advisable to assess renal function prior to initiating loop therapy and to schedule electrolyte panels within the first 48 hours of treatment.
Should hypokalemia emerge, adjunctive therapy with a potassium‑sparing diuretic can be introduced in a stepwise fashion.
Patient education on signs of dehydration and auditory changes enhances safety and promotes adherence.
By integrating these measures, the therapeutic benefits of furosemide can be maximized while minimizing adverse outcomes.
Madhav Dasari
October 20, 2025 AT 22:23Hey folks, just wanted to throw in a quick pep talk – if you’re juggling diuretics, remember you’ve got options! A loop like furosemide gets the job done fast, but if you need something that sticks around longer, give torsemide a shout.
Don’t forget to pair with a potassium‑spare if the labs start looking low – it’s a simple tweak that makes a huge difference.
Stay optimistic, keep monitoring, and you’ll find the sweet spot for each patient.
Jameson The Owl
October 21, 2025 AT 06:43When one examines the ontogeny of loop diuretic utilization one must first acknowledge the historical predilection for furosemide as the archetype of rapid volume off‑loading.
The mechanistic underpinnings involve a high‑affinity blockade of the NKCC2 transporter within the thick ascending limb, a locus of considerable reabsorption capacity.
Consequently the resultant osmotic diuresis is precipitous, often effectuating a measurable reduction in pulmonary congestion within minutes.
Yet the pharmacodynamic landscape is not monolithic; bumetanide, possessing roughly 1.3‑times the potency per milligram, offers a concentration‑dependent alternative wherein lower mass yields comparable natriuresis.
This potency differential becomes clinically salient when fluid overload threatens renal perfusion and physician stewardship demands dosage minimization.
Torsemide, by contrast, extends its half‑life to approximately twelve hours, furnishing a steadier diuretic curve that mitigates the peaks and troughs observed with furosemide boluses.
The anti‑aldosterone properties ascribed to torsemide further augment its utility in heart‑failure cohorts by attenuating neurohormonal activation.
From a safety perspective, the ototoxic risk profile of high‑dose furosemide is non‑trivial; cochlear hair cell susceptibility escalates in proportion to serum concentration and infusion velocity.
Clinical vigilance demands that infusion rates be throttled to sub‑bolus velocities, or that alternative loops be considered in predisposed individuals.
Electrolyte disturbances, notably hypokalemia, are an inevitable sequela of loop therapy, necessitating either supplemental potassium or the strategic addition of a potassium‑sparing agent such as spironolactone.
However, the latter brings its own specter of hyperkalemia, particularly in the setting of concomitant renal insufficiency, thereby mandating serial monitoring of serum potassium and creatinine.
Cost considerations cannot be ignored; while furosemide and hydrochlorothiazide are generically inexpensive, the newer loops command higher acquisition costs, a factor that may influence formulary decisions in resource‑constrained settings.
Nevertheless, the potential for reduced hospital length of stay with more effective diuresis may offset these expenditures when viewed through a health‑economic lens.
Prescribing algorithms should therefore integrate patient‑specific variables: eGFR, volume status, comorbid hypertension, and susceptibility to electrolyte derangements.
In summary, the clinician’s armamentarium includes a spectrum of diuretics, each with distinct pharmacokinetic and pharmacodynamic attributes, and the optimal selection hinges upon a composite assessment of urgency, duration, renal function, and safety profile.
Rakhi Kasana
October 21, 2025 AT 15:03The comparative table is helpful but it glosses over the subtleties of patient‑centred decision making.
For instance, the assertion that torsemide’s anti‑aldosterone effect is universally beneficial ignores the potential for hyperkalemia in borderline renal function.
Moreover, the cost discussion omits consideration of insurance formularies that may restrict access to certain loops.
A more granular approach would weigh these contextual factors alongside the pharmacologic data.
Sarah Unrath
October 21, 2025 AT 23:23Grea info!
Christian Georg
October 22, 2025 AT 07:43Interesting points about the ototoxic risk, especially for patients on high‑dose IV furosemide 😊.
In practice, I’ve found that slowing the infusion rate to 20 mg over 30 minutes can markedly reduce hearing complaints while still achieving diuresis.
Also, pairing a low‑dose loop with a thiazide in resistant edema can exploit synergistic natriuresis without excessive potassium loss.
Christopher Burczyk
October 22, 2025 AT 16:03While the mitigation strategies outlined are pragmatic, it is essential to underscore that any alteration in diuretic regimen must be predicated on serial laboratory assessment.
Specifically, serum potassium and creatinine should be re‑checked within 24 hours of any dosage modification to preempt iatrogenic complications.
This systematic approach ensures therapeutic efficacy without compromising patient safety.
Caroline Keller
October 23, 2025 AT 00:23This whole diuretic debate feels like a soap opera and honestly it’s exhausting to read endless tables when patients just need clear guidance.
We need simple takeaways, not a dissertation of side‑effects that leaves everyone confused.