Heat Risk Medication Checker
Medication Heat Risk Assessment
Check your risk of heat intolerance based on medications you're taking. This tool helps identify dangerous medication combinations that may affect your body's ability to regulate temperature.
When the temperature rises, your body sweats to cool down. It’s simple biology. But if you’re taking certain medications, that natural cooling system can shut down - not because your body is broken, but because the drugs you’re taking are interfering with it. This isn’t rare. It’s common. And it’s dangerous.
Why Some Medications Make You Overheat
Your body regulates temperature through three main tools: sweating, blood flow to the skin, and fluid balance. When any of these get disrupted, your core temperature climbs. And that’s when heat intolerance kicks in. Some drugs block the nerves that tell your sweat glands to activate. Others reduce how much blood reaches your skin, trapping heat inside. Some make you pee so much you become dehydrated, leaving your body with no water to sweat. And a few even trick your brain into thinking you’re not thirsty, even when you’re dangerously dry. This isn’t just about discomfort. Heat intolerance can lead to heat exhaustion - and then heat stroke. Heat stroke kills. The CDC reports that untreated heat stroke has a mortality rate between 10% and 65%. If you’re on medication that affects your body’s ability to cool itself, you’re at higher risk.Top Medication Classes That Cause Heat Intolerance
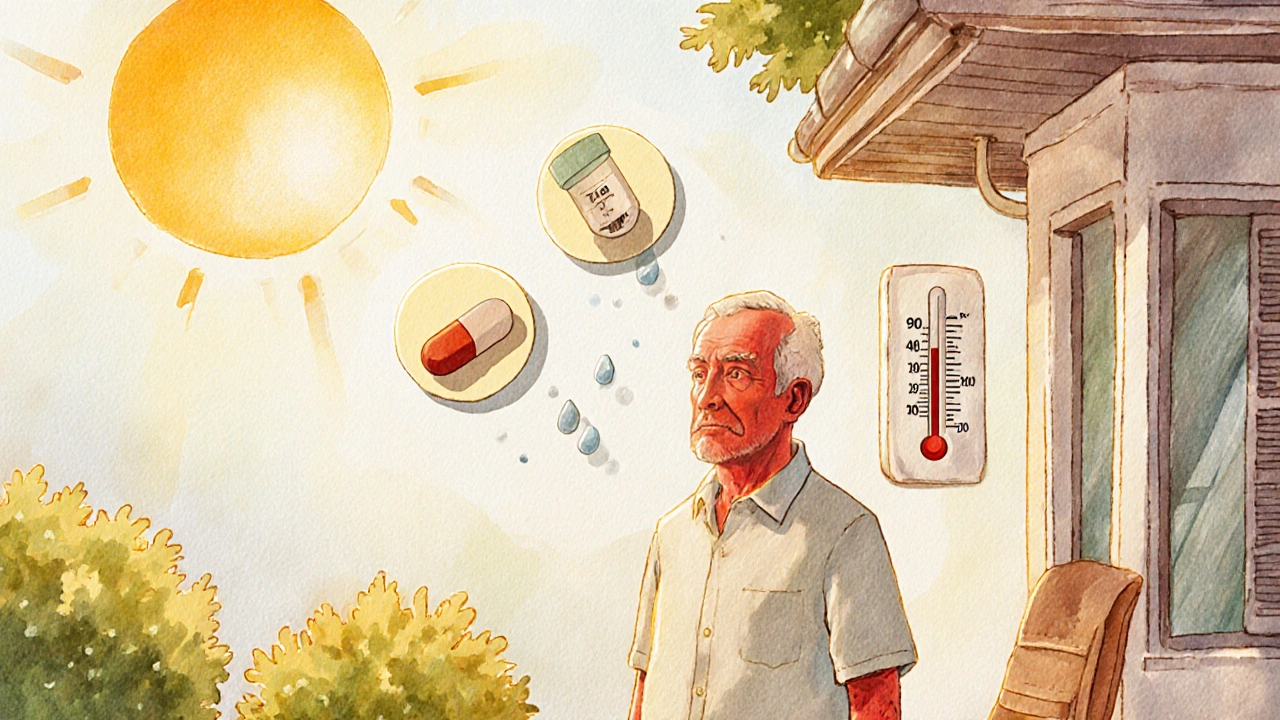
There are 14 known classes of medications that can interfere with thermoregulation. But five stand out as the biggest culprits.- Diuretics - These are often called "water pills." They’re used for high blood pressure and heart failure. Common ones include hydrochlorothiazide and chlorthalidone. They force your kidneys to dump 1-2 liters of fluid a day. That’s a lot. Less fluid means less sweat. Studies show diuretics can cut your sweating capacity by 30-50%. In July and August heat waves, people on hydrochlorothiazide have 2.3 times the risk of heat exhaustion.
- Beta blockers - Used for heart conditions, anxiety, and migraines. Drugs like metoprolol and propranolol reduce blood flow to the skin by 25-40%. That means heat can’t escape. Your skin stays cool, but your core temperature rises. Non-selective beta blockers like propranolol are worse than selective ones like metoprolol, because they affect more blood vessels.
- Anticholinergics - These include overactive bladder meds like oxybutynin, allergy pills like diphenhydramine (Benadryl), and some antidepressants. They block acetylcholine, the chemical that tells sweat glands to work. This can reduce sweating by 60-80%. Many people don’t realize their dry skin and heat sensitivity are from a nightly sleep aid.
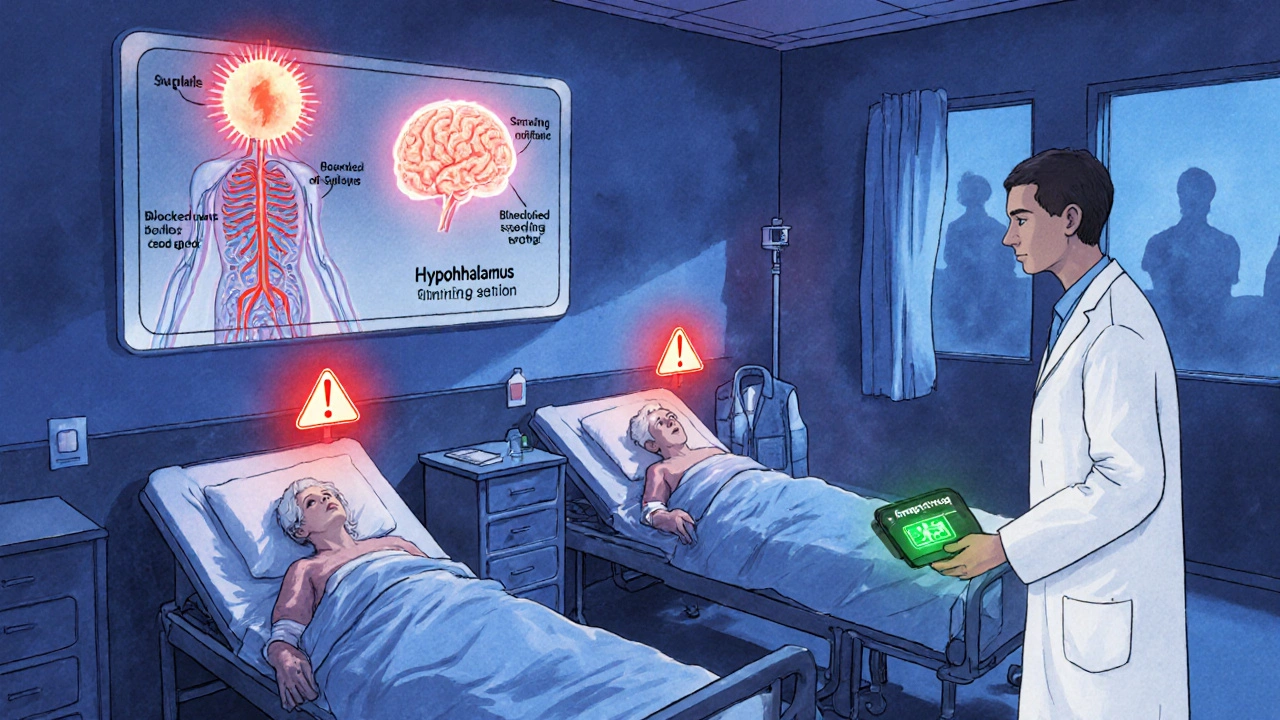
- Antipsychotics - Medications like olanzapine, quetiapine, and haloperidol are among the most dangerous. They don’t just reduce sweating - they disrupt the hypothalamus, the part of your brain that controls body temperature. This means you can develop heat stroke even when it’s only 27-32°C (80-90°F). The CDC lists these as top-tier risks.
- GLP-1 receptor agonists - These are the weight-loss drugs like semaglutide (Ozempic, Wegovy). They suppress thirst by 40-50%. You might drink plenty of water, but your brain doesn’t tell you to drink more. Dehydration creeps up silently. Dr. Nish Shah from Houston Methodist warns that this is a hidden danger for people who think they’re "being healthy" by losing weight.
What About Antidepressants?
Not all antidepressants are the same when it comes to heat. Tricyclic antidepressants - like amitriptyline and clomipramine - reduce sweating by 65-75%. They’re anticholinergic, so they work the same way as Benadryl. But SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) do the opposite. They can actually make you sweat more. That sounds good - until you realize you’re losing fluids faster than you can replace them. So even if you’re sweating, you’re still at risk for dehydration and heat illness.Stimulants and ADHD Medications
Ritalin, Adderall, and other stimulants increase your metabolic rate by 15-25%. That means your body is burning more energy - and generating more heat. At the same time, they can reduce blood flow to the skin and impair sweating. The result? You’re overheating from the inside out. The good news? Atomoxetine (Strattera), a non-stimulant ADHD medication, has little to no effect on thermoregulation. If you’re on stimulants and live in a hot climate, talk to your doctor about alternatives.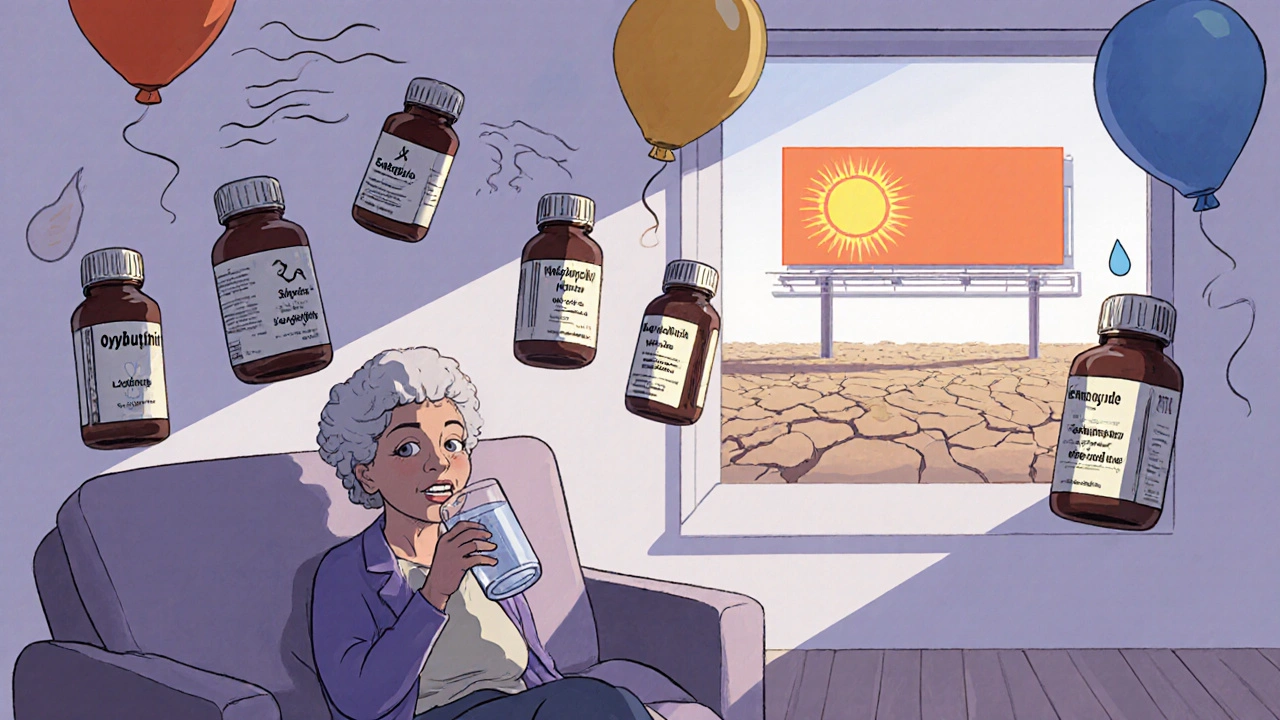
Signs You’re Overheating
You don’t need to wait for heat stroke to realize something’s wrong. Early signs show up fast - often within 30 to 90 minutes of being in the heat.- Cramps in your arms, legs, or stomach (65% of cases)
- Dizziness or lightheadedness (55%)
- Headache (70%)
- Flushed, red skin
- Feeling unusually tired or weak (60%)
- Nausea or vomiting (35%)
- Either excessive sweating - or no sweating at all (85% of cases)
Who’s Most at Risk?
It’s not just about the drug. It’s about how many you’re taking. People over 65 are especially vulnerable. Their bodies naturally sweat less. Their thirst signals weaken. And they’re more likely to be on multiple medications. The American Geriatrics Society says that taking five or more medications increases your risk of heat stroke by 300% compared to younger, healthier adults. That’s not a small number. That’s a red flag. Even more concerning: people on three or more heat-affecting drugs account for 18-22% of all heat-related ER visits among adults over 50. If you’re on diuretics, an anticholinergic, and a beta blocker? You’re in the danger zone.What You Can Do
You don’t have to stop your meds. But you do need to manage the risk.- Drink more water - Add 500-1000 mL (about 2-4 cups) to your daily intake during hot weather. Don’t wait until you’re thirsty.
- Avoid the sun - Stay indoors between 10 a.m. and 4 p.m. That’s when UV radiation is strongest and temperatures peak.
- Use air conditioning - If your home doesn’t have AC, go to a library, mall, or community center. Even a few hours of cooling can reset your body.
- Monitor your weight - A drop of more than 2% in your body weight over a day means you’re dehydrated. Weigh yourself in the morning, before eating or drinking.
- Use cooling gear - For people on antipsychotics or anticholinergics, cooling vests can lower core temperature by 0.5-1.0°C. That’s enough to prevent heat stroke.
- Check your meds - Ask your doctor or pharmacist: "Could any of these drugs make me more sensitive to heat?" Don’t assume they know. Many don’t.
Special Cases: Lithium and Skin Sensitivity
Lithium, used for bipolar disorder, is especially risky. It has a narrow therapeutic range - meaning the difference between a helpful dose and a toxic one is small. When you’re dehydrated, your lithium levels can spike by 25-35%. That can cause tremors, confusion, seizures, or even kidney damage. The CDC says lithium patients need their blood levels checked during heat waves - especially when temperatures go above 29°C (85°F). Also, some blood pressure drugs - like calcium channel blockers, ACE inhibitors, and ARBs - can make your skin more sensitive to the sun. Use SPF 30+ sunscreen daily, even if you’re just walking to your car.The Bigger Picture
This isn’t just a personal health issue. It’s a public health crisis. 2023 was the hottest year on record. By 2050, heat-related complications from medications could increase by 40-60% if current climate trends continue. Hospitals are already seeing more cases. Emergency rooms are overwhelmed. Elderly patients are dying. New tools are emerging. The FDA approved a wearable core temperature monitor called TempTraq in December 2023 - the first device designed specifically for people on heat-sensitive medications. Electronic health records now flag high-risk drug combinations during summer months. But the most powerful tool is still knowledge. If you’re on any of these medications, you need to understand how they affect your body. You need to know the signs. You need to plan ahead.Frequently Asked Questions
Can I stop my medication if it makes me sensitive to heat?
Never stop a medication without talking to your doctor. Many of these drugs treat life-threatening conditions like high blood pressure, heart disease, or mental illness. Stopping suddenly can be dangerous. Instead, work with your provider to adjust your plan - maybe switch to a different drug, change your dose, or add safety measures like cooling vests or more frequent hydration.
Do all antihistamines cause heat intolerance?
No. Only older, first-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine have strong anticholinergic effects. Newer ones like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) don’t affect sweating and are safer in hot weather.
Is it safe to exercise if I’m on heat-sensitive meds?
It depends. Avoid outdoor exercise during peak heat hours. If you want to stay active, try indoor workouts in air-conditioned spaces - swimming, cycling on a stationary bike, or walking on a treadmill. Always hydrate before, during, and after. If you feel dizzy, nauseous, or unusually tired, stop immediately. Your body is signaling danger.
Can drinking more water prevent heat stroke from medications?
It helps - but it’s not enough. If your sweat glands are blocked by anticholinergics, or your blood vessels won’t dilate because of beta blockers, drinking water won’t fix the root problem. Hydration is one part of a bigger plan. You also need to avoid heat, use cooling tools, and monitor your symptoms.
Are there any medications that help with heat intolerance?
No. There are no drugs designed to reverse medication-induced heat intolerance. Treatment focuses on prevention: hydration, cooling, avoiding heat, and sometimes switching medications. Research is underway for heat-resistant drug formulations, but none are available yet.
Should I wear a medical alert bracelet if I’m on these meds?
If you’re on multiple heat-sensitive medications - especially antipsychotics, lithium, or diuretics - yes. In an emergency, first responders may not know your full medication list. A bracelet that says "Heat Sensitive: On Anticholinergics & Diuretics" could save your life.
Katelyn Sykes
November 17, 2025 AT 07:55Just found out my nightly Benadryl for sleep is making me sweat less. No wonder I feel like a furnace at night. Switched to Zyrtec and already feel cooler. Why don't doctors tell you this stuff?
Also, if you're on anything anticholinergic, stop using those cooling wristbands. They don't do jack if your glands are shut down.
Gabe Solack
November 18, 2025 AT 04:27Bro I was just telling my aunt this yesterday. She’s on hydrochlorothiazide and propranolol and thought her fatigue was just aging. Turned out she was one heat wave away from the ER.
She got a cooling vest and now she’s gardening again 🙌
Also, if you’re on GLP-1s, drink water like it’s your job. Your brain’s lying to you.
Denny Sucipto
November 19, 2025 AT 04:06Man, I didn’t think twice about my olanzapine until my cousin passed out at a BBQ last summer. He was 42. No preexisting conditions. Just meds and heat.
Now I carry a little digital thermometer in my pocket. If my core hits 100.5, I’m inside. No excuses.
Also, if you’re on lithium? Don’t even think about skipping water. That shit can turn your brain into mush real quick.
Sarah Frey
November 19, 2025 AT 18:41Thank you for this meticulously researched and clinically vital summary. The integration of epidemiological data with pharmacological mechanisms is both rigorous and accessible. I would strongly encourage healthcare institutions to implement mandatory patient counseling protocols regarding thermoregulatory risks associated with polypharmacy, particularly during seasonal heat advisories. This is not merely an individual concern-it is a systemic public health imperative requiring interdisciplinary coordination.
Holly Powell
November 20, 2025 AT 21:34Actually, the real issue here is the lack of pharmacogenomic screening. We’re treating thermoregulatory dysfunction as a side effect when it’s a CYP450-mediated phenotype expression. The FDA’s passive surveillance system is archaic. We need real-time pharmacovigilance dashboards linked to EHRs and ambient temperature APIs. This isn’t ‘awareness’-it’s a failure of precision medicine infrastructure.
Yash Nair
November 21, 2025 AT 06:10USA is so weak. In India we dont care about heat. We sweat all day and take 5 meds at once. You people are soft. Drink chai and walk in sun. No AC no problem. Why you need vest? LOL. Also why you take so many pills? Just eat turmeric and chill.
Emanuel Jalba
November 22, 2025 AT 23:19THIS IS A GOVERNMENT CONSPIRACY. They want us to be weak so we stay inside and don’t protest. The FDA knows these drugs cause heat stroke but they let it happen because they’re paid by Big Pharma. They even made the TempTraq so you think you’re safe but it’s just a tracker for your data. I saw a guy in a hoodie in 90 degree heat with a vest. He was crying. He knew. 😢💊🔥
Kristina Williams
November 24, 2025 AT 06:44My neighbor’s dog got heat stroke last year. He was on Zoloft. Coincidence? I don’t think so. I think the government is using antidepressants to control the population. If you sweat less you’re less likely to go outside and protest. That’s why they made SSRIs make you sweat too-it’s a trap. You think you’re cool but you’re dehydrated. It’s all connected.
Shilpi Tiwari
November 24, 2025 AT 13:34From a pharmacokinetic standpoint, the CYP2D6 polymorphism significantly modulates the anticholinergic burden of first-generation H1 antagonists. The reduced sweat gland density in elderly populations, compounded by diminished aquaporin-5 expression, creates a nonlinear risk gradient. I’d argue that current guidelines underrepresent the interaction between polypharmacy and thermoregulatory gene expression-particularly in South Asian cohorts where baseline hydration thresholds differ.
Bailey Sheppard
November 24, 2025 AT 13:51Thanks for sharing this. I’ve been on metoprolol for years and never realized my skin staying cool was a warning sign. I started drinking more water and now I take walks in the early morning. Feels good to be proactive. No drama, just care.
Also, if you’re on meds and feel off in the heat, don’t ignore it. Just pause. Breathe. Sit down. You’ve got this.
Kristi Joy
November 26, 2025 AT 00:17I’m a nurse and I’ve seen too many elderly patients come in with heat stroke because they didn’t know their meds were the problem. One lady was on 7 drugs including oxybutynin and hydrochlorothiazide. She thought her dizziness was just old age.
Now I hand out little cards to every patient on these meds: "Heat = Danger. Water = Lifeline. Shade = Sanctuary." Simple. Clear. Maybe it saves someone.
You’re not weak for needing help. You’re smart for asking.
Heidi R
November 26, 2025 AT 03:02So basically, if you're not rich enough to afford a cooling vest, you're just supposed to die in the heat? And your doctor doesn't care? Classic.
Louie Amour
November 26, 2025 AT 11:56Wow, this post is so basic. Anyone with a PubMed account could’ve written this. The real issue is that people don’t understand physiology. You can’t just ‘drink more water’-you need to optimize electrolyte balance via sodium-potassium co-transport modulation. Also, your mention of GLP-1s is laughably incomplete. You didn’t even touch on the vagal nerve suppression mechanism. Amateur hour.