Itching that won’t go away - no matter how much you scratch - is one of the most frustrating symptoms of liver disease. In cholestasis, where bile doesn’t flow properly, this itch isn’t caused by dry skin or allergies. It’s driven by chemicals building up in your blood, especially bile acids and a molecule called lysophosphatidic acid (LPA). For decades, doctors turned to cholestyramine, a bile acid resin, as the first-line fix. But it’s gritty, tastes awful, and doesn’t work for everyone. Now, newer drugs are changing the game.
Why Does Cholestasis Cause Itching?
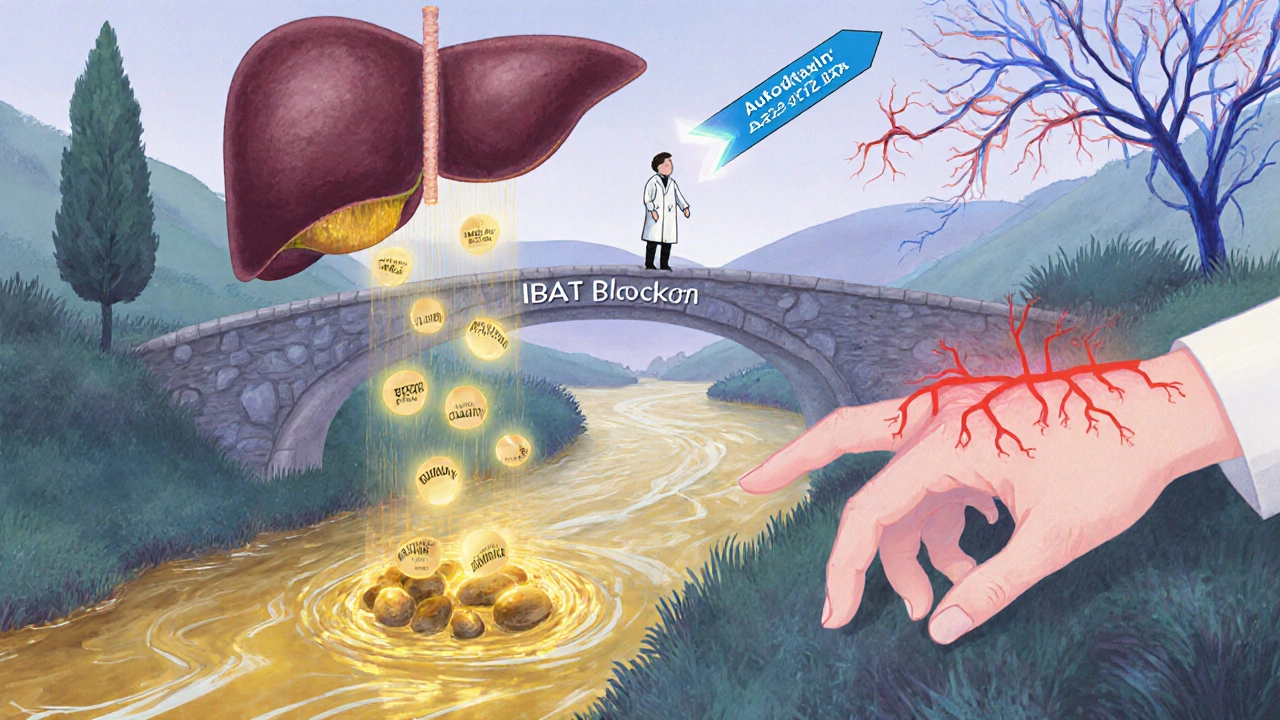
Cholestasis means bile isn’t moving the way it should. Whether it’s from primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), or pregnancy-related cholestasis, the liver can’t clear out bile components. These compounds - especially bile acids - get trapped in the bloodstream. But here’s the twist: it’s not just bile acids causing the itch. Research since 2016 points to autotaxin, an enzyme that makes LPA, as a key player. LPA directly activates nerve fibers in the skin, triggering that relentless itch. That’s why antihistamines, which work for allergic itching, almost never help here. The AASLD guidelines clearly state: don’t waste time on them.
Cholestyramine: The Old Standard, With Big Drawbacks
Cholestyramine (brand name Questran) has been around since the 1960s. It’s a resin that binds bile acids in your gut, so they’re flushed out in stool instead of being reabsorbed. Dosing starts at 4 grams once a day, and can go up to 16-24 grams daily, split into doses. For about half to two-thirds of patients, it cuts itching by 50-70%. Sounds good - until you try it.
The powder is chalky, gritty, and tastes like wet sand. Most people can’t tolerate it long-term. A 2021 survey of 342 patients found 65% stopped using it within three months. Even worse, it binds to other medications - antibiotics, thyroid pills, birth control - so you have to take it one hour before or four to six hours after everything else. That’s a logistical nightmare. Still, it’s the first step because it’s cheap ($65 a month) and has decades of safety data. But if you’re not getting relief after four weeks, it’s time to move on.
Rifampin: The Second-Line Powerhouse
If cholestyramine fails, rifampin (Rifadin) is next. It’s an antibiotic, but in this case, it’s not fighting infection. Rifampin turns on liver enzymes that help process and eliminate pruritogens - the itch-causing substances - faster. Dosed at 150-300 mg daily, it works in about 70% of PBC patients within four weeks. One patient on Reddit wrote: “Rifampin turned my urine orange but dropped my itching from 8/10 to 3/10 in two weeks.”
But it’s not perfect. About 15-20% of users develop elevated liver enzymes, so liver function tests must be monitored. It also interacts with over 50 other drugs because it speeds up how fast your liver breaks them down. Birth control, blood thinners, and even some antidepressants can become less effective. Still, for many, the trade-off is worth it. Discontinuation rates are low - only 10-15% - compared to cholestyramine’s 35%.
Naltrexone and Sertraline: Targeting the Nervous System
When bile acid binders and rifampin don’t cut it, doctors look at the brain and nerves. Naltrexone, used for opioid addiction, blocks the same receptors that may be overstimulated by endogenous opioids in cholestasis. Dosed at 12.5-50 mg daily, it helps 50-60% of patients. But starting it is rough. About 30% report nausea, anxiety, and flu-like symptoms in the first few days - like opioid withdrawal, even if they’ve never used opioids. That’s why doctors start low: 6.25 mg, then increase weekly.
Sertraline (Zoloft), an SSRI antidepressant, is used off-label. It’s less about mood and more about serotonin’s role in itch signaling. In PBC patients, it reduces itching in 40-50% of cases. It’s gentler than naltrexone but only works well in PBC, not PSC or other forms. It’s a good option if depression or anxiety is also part of the picture.
New Hope: Maralixibat and the Future of Targeted Therapy
The biggest shift in the last five years is moving from broad treatments to targeted ones. Maralixibat (Mytesi), approved by the FDA in 2021 for Alagille syndrome, blocks the ileal bile acid transporter (IBAT). That stops bile acids from being reabsorbed in the gut - similar to cholestyramine, but as a pill, not a powder. In the phase 3 MARCH trial, it reduced itch by 47% on a visual scale, nearly matching cholestyramine’s 42%. But here’s the game-changer: 82% of patients kept taking it at six months. Only 12% quit, compared to 35% with cholestyramine.
Patients love it. No grit. No taste. Once-daily dosing. Side effects are mild - mostly loose stools. But the cost? Around $12,500 a month. That’s a huge barrier. Still, it’s a sign of things to come. Other IBAT inhibitors like volixibat are in phase 3 trials, showing 52% itch reduction. And the most exciting frontier? Drugs that block autotaxin, the enzyme that makes LPA. IONIS-AT332-LRx, an antisense oligonucleotide, cut serum autotaxin by 65% and pruritus by 58% in a 2023 trial. That’s not just symptom relief - it’s targeting the root cause.
When Nothing Else Works: Transplant and Other Options
For the 10-15% of patients who don’t respond to any medical therapy, liver transplant remains the only cure. Post-transplant, 95% of patients report complete resolution of itching. But it’s major surgery, with lifelong risks and medication requirements. It’s reserved for advanced disease or unbearable quality of life.
For those with extrahepatic obstruction - a blocked bile duct from a stone or tumor - stent placement can offer immediate relief. One expert notes that 85% of these patients get significant itch reduction right after the procedure. Yet, many clinicians still overlook this option, focusing only on drugs.
What Works Best - And When
There’s no one-size-fits-all. Here’s what the evidence says:
- First step: Cholestyramine 4g daily, titrated up over two weeks. Add emollients, cool showers, loose cotton clothes.
- If no improvement in 4 weeks: Add rifampin 150mg daily, increase to 300mg if tolerated.
- If still no relief: Try naltrexone (start at 6.25mg) or sertraline (50-100mg).
- If you can afford it and have Alagille or severe PBC: Maralixibat is the best-tolerated option with strong data.
- Always: Avoid antihistamines. They don’t work. And never combine cholestyramine with other meds without timing them properly.
Doctors in academic centers follow this stepwise approach 78% of the time. In community practices? Only 45%. That gap means many patients suffer longer than they need to. If your doctor keeps prescribing hydroxyzine or diphenhydramine for your liver itch, ask why. The guidelines are clear: it’s not histamine.
The Road Ahead
The future of cholestatic pruritus treatment is precise. We’re moving from guessing what’s causing the itch to knowing exactly which pathway to block. Autotaxin inhibitors, IBAT blockers, and even repurposed drugs like GLP-1 agonists (which unexpectedly reduced itch in diabetic PBC patients) are reshaping care. Within five years, most patients won’t be swallowing chalky powders. They’ll be on targeted pills that stop the itch at its source.
But access remains a problem. Maralixibat costs over $12,000 a month. Cholestyramine costs $65. That’s not just a price difference - it’s a health equity issue. Until these new drugs become affordable or generics emerge, many will still be stuck with the old, imperfect options.
For now, the key is persistence. Don’t give up after one failed treatment. Work with your hepatologist. Track your itch on a scale of 1 to 10. Keep a log of what helps and what doesn’t. You’re not alone - over 1.5 million Americans live with cholestatic liver disease. And the treatments are getting better, faster than ever before.
Why don’t antihistamines work for cholestatic itching?
Antihistamines block histamine, a chemical involved in allergic reactions and skin irritation. But cholestatic pruritus isn’t caused by histamine. It’s triggered by bile acids, lysophosphatidic acid (LPA), and endogenous opioids building up in the blood and stimulating nerve endings directly. Multiple studies, including those from the American Association for the Study of Liver Diseases (AASLD), confirm that antihistamines have no meaningful effect on this type of itch - yet they’re still prescribed by 68% of primary care doctors due to outdated habits.
Can I take cholestyramine with my other medications?
No, not at the same time. Cholestyramine binds to many drugs in the gut, preventing them from being absorbed. This includes antibiotics, thyroid hormones, birth control pills, warfarin, and many others. To avoid interactions, take cholestyramine at least one hour before or four to six hours after any other medication. Always check with your pharmacist or hepatologist before starting or changing any drug while on cholestyramine.
Is rifampin safe for long-term use in cholestasis?
Rifampin is generally safe for long-term use in cholestatic pruritus, but liver enzymes must be monitored every 2-4 weeks, especially in the first few months. About 15-20% of patients develop mild elevations in liver enzymes, which usually resolve with dose reduction or stopping the drug. It’s not addictive and doesn’t cause liver damage directly, but its effect on liver metabolism means it can interfere with other medications. If you’re on birth control, blood thinners, or antivirals, your doctor needs to adjust those doses accordingly.
How does maralixibat compare to cholestyramine?
Maralixibat works similarly to cholestyramine by blocking bile acid reabsorption - but it’s a pill, not a powder. It reduces itching by about 47% in clinical trials, nearly matching cholestyramine’s 42%. The big difference is tolerability: 82% of patients stay on maralixibat after six months, compared to only 45% for cholestyramine. Side effects are milder (mostly diarrhea), and there’s no taste or texture issue. However, maralixibat costs about $12,500 per month, while cholestyramine is under $70. Insurance coverage varies widely.
Are there any new drugs coming for cholestatic pruritus?
Yes. Volixibat, another IBAT inhibitor, showed 52% itch reduction in phase 3 trials. The most promising are autotaxin inhibitors like IONIS-AT332-LRx, which target the root cause - lysophosphatidic acid (LPA) production. In a 2023 trial, it cut serum autotaxin by 65% and pruritus by 58%. GLP-1 agonists, used for diabetes, also unexpectedly reduced itching in PBC patients, suggesting new repurposing opportunities. These drugs are in late-stage trials and could be available within the next 2-4 years.
What to Do Next
If you’re living with cholestatic pruritus and current treatments aren’t working, don’t accept it as inevitable. Talk to your hepatologist about stepping up therapy. Keep a daily itch log - rate it from 1 to 10, note triggers, and track what helps. Ask if you’re a candidate for maralixibat or if clinical trials for newer drugs are open. Bring up stent placement if you have bile duct obstruction. And if your doctor still prescribes antihistamines, ask for the evidence. You deserve better than a dusty powder that tastes like chalk. The future of treatment is here - you just need to ask for it.

Sheldon Bazinga
November 20, 2025 AT 09:17Chris Vere
November 20, 2025 AT 16:21Leo Tamisch
November 21, 2025 AT 12:02Clifford Temple
November 22, 2025 AT 08:02Corra Hathaway
November 23, 2025 AT 19:46Paula Jane Butterfield
November 23, 2025 AT 21:15Simone Wood
November 25, 2025 AT 19:26Steve Harris
November 26, 2025 AT 11:39Cooper Long
November 27, 2025 AT 16:22Sandi Moon
November 29, 2025 AT 01:41Kartik Singhal
November 29, 2025 AT 17:21Logan Romine
November 30, 2025 AT 20:53