When you suddenly see a shower of new floaters, or a flash of light out of the corner of your eye, it’s easy to brush it off. Maybe it’s just eye strain. Maybe you’re tired. But if you’re over 40, nearsighted, or had cataract surgery, that moment could be your last chance to save your vision. Retinal detachment doesn’t wait. It doesn’t come with warning signs you can ignore. And if you delay treatment even a few hours, your chances of keeping clear vision drop fast.
What Happens When the Retina Detaches
The retina is the thin, light-sensitive layer lining the back of your eye. It’s like the film in a camera-when light enters your eye, the retina captures the image and sends it to your brain. If it pulls away from its blood supply, the cells start dying. That’s retinal detachment. And once those photoreceptor cells die, they don’t come back. It’s not a slow fade. It’s sudden. And it’s silent. You won’t feel pain. No redness. No swelling. Just vision changes that feel weird but not scary-until they’re too late.The Six Emergency Symptoms You Must Recognize
There are six clear warning signs that mean you need to see a specialist today, not tomorrow.- Sudden increase in floaters-not one or two, but dozens, or even a cloud of dark specks or squiggly lines that won’t go away. This isn’t the occasional floater you’ve had for years. This is new, fast, and overwhelming.
- Flashes of light-like camera strobes in your peripheral vision, especially in the dark. These aren’t afterimages from bright lights. They’re persistent, brief bursts that feel like electricity in your eye.
- A dark curtain or shadow-this is the most urgent sign. It starts in your side vision and creeps inward, like a shade being pulled across your field of view. If it reaches the center, you’re losing central vision.
- Blurry or distorted vision-everything looks warped, wavy, or out of focus, even with glasses. This often means the macula, the part responsible for sharp vision, is starting to detach.
- Loss of peripheral vision-you can’t see things out of the corner of your eye. You bump into doorframes. You miss people walking up beside you.
- Sudden color changes-colors look duller, washed out, or shifted. This happens when the macula is involved. It’s rare, but when it happens, it’s a red flag.
If you have even one of these symptoms, especially if they came on suddenly, go to an eye doctor immediately. Don’t wait. Don’t call your primary care provider first. Go straight to an ophthalmologist or an emergency eye clinic. The average patient waits 48 hours before seeking help-and that’s too long.
How Doctors Diagnose a Detached Retina
There’s no blood test or X-ray for this. Diagnosis requires a detailed eye exam using specialized tools. The gold standard is a dilated fundus examination. The doctor uses a bright light and a special lens (like a 20D or 90D lens) to look deep into your eye. They’ll see if the retina is wrinkled, folded, or completely lifted off the back wall. If your eye is cloudy from a cataract or bleeding, they’ll use B-scan ultrasound-a small probe placed gently on your eyelid sends sound waves to create an image of the retina. It’s quick, painless, and tells them exactly where the detachment is. They may also use optical coherence tomography (OCT), which gives a high-resolution cross-section of the retina. It shows if fluid is under the retina, how thick it is, and whether the macula is still attached. These aren’t tools your regular optometrist has in their office. That’s why many patients get misdiagnosed as having “eye strain” or “migraine aura.” Only a retina specialist or emergency eye clinic has the right equipment and experience to catch this early.The Three Main Surgical Treatments
There are three main surgeries to fix a detached retina. Which one you get depends on where the tear is, how big it is, and whether your macula is still attached.1. Pneumatic Retinopexy
This is the least invasive. The doctor injects a gas bubble into your eye. Then, you have to position your head so the bubble floats up and presses against the retinal tear, sealing it. A laser or freezing treatment is used to glue the retina back in place. It works best for small, single tears on the top of the retina. Success rate: 70-80%. But if the tear is on the bottom, it won’t work-the bubble floats up, not down. The downside? You have to stay in a face-down or side-lying position for 50 out of every 24 hours for 7-10 days. That’s hard. You can’t read, watch TV, or cook. Many people need help eating, bathing, and using the bathroom.2. Scleral Buckling
This is a more traditional method. A soft silicone band is sewn around the outside of your eye, gently pushing the wall inward to meet the detached retina. It’s like putting a belt around your eye to hold things in place. It’s very effective for younger patients, especially those with lattice degeneration or severe nearsightedness. Success rate: 85-90%. But it can change your vision. Many people develop new nearsightedness (1.5-2.0 diopters) and some get double vision. Recovery takes weeks.3. Vitrectomy
This is the most common surgery today-used in about 65% of cases. The surgeon removes the gel-like vitreous from inside your eye and replaces it with a gas or silicone oil bubble. Then they use a laser to seal the tear. It’s the go-to for complex cases: large tears, multiple breaks, or if the macula is already detached. Success rate: 90-95%. But there’s a catch: if you still have your natural lens, you’ll likely develop a cataract within two years. About 70% of patients need cataract surgery after vitrectomy. You’ll also need to stay face-down after surgery if gas is used. Silicone oil doesn’t require positioning, but it has to be removed in a second surgery months later.Time Is Everything
The single biggest factor in your vision outcome? How fast you get treated. If your macula is still attached when surgery happens, you have a 90% chance of keeping 20/40 vision or better. That’s good enough to drive, read, and live normally. But if the macula has detached, your vision drops fast. Every hour counts. Studies show you lose about 5% of your potential vision recovery for every hour you wait. After 72 hours, your chance of getting back 20/40 vision drops from 75% to just 35%. That’s why top hospitals like Wills Eye have protocols: if the macula is off, you get evaluated within 4 hours and operated on within 12. No delays. No waiting for insurance approval. This is an emergency, not an appointment.Who’s at Risk?
You’re at higher risk if you:- Are nearsighted (more than -5.00 diopters)-your retina is thinner and stretched
- Have had cataract surgery-risk increases 0.5% to 2%
- Have lattice degeneration-a thinning of the retina common in younger people
- Have a family history of retinal detachment
- Have had an eye injury or previous retinal detachment in the other eye
It affects about 1 in 10,000 people each year-but that number jumps to 20 in 10,000 if you’re over 40. And for those with severe nearsightedness, it’s 167 in 10,000. That’s not rare. It’s a real threat.
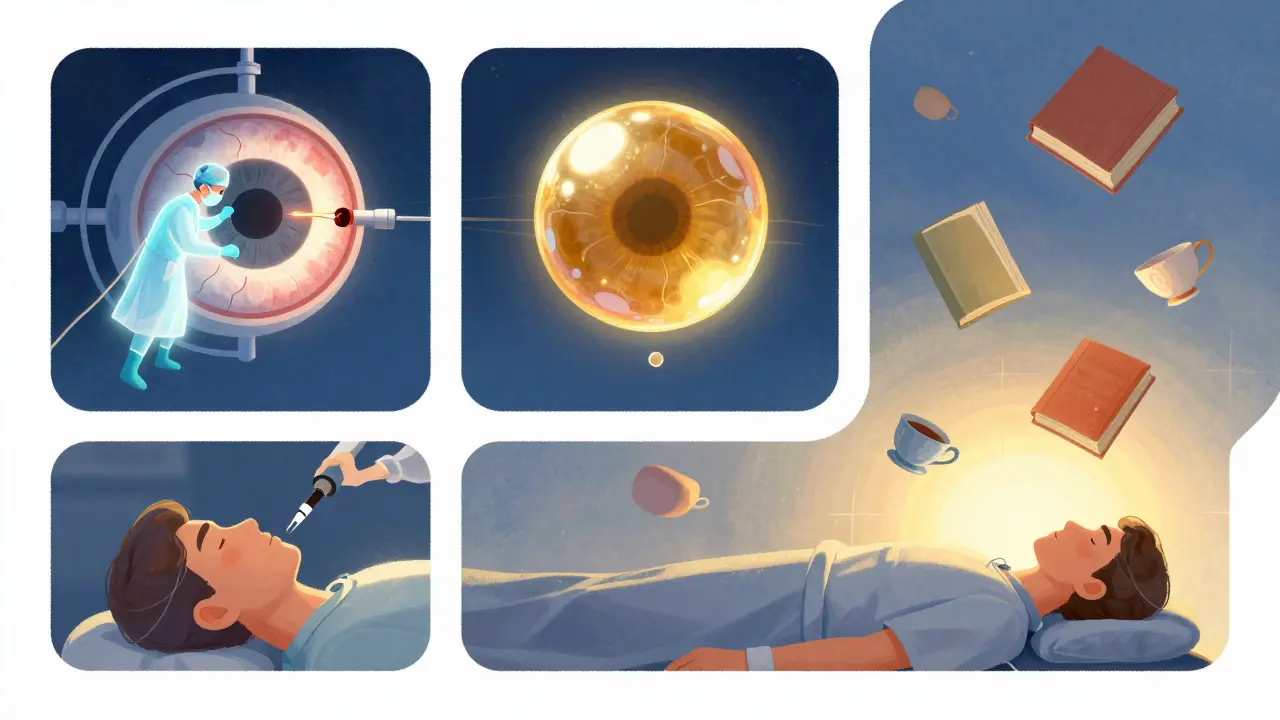
What Happens After Surgery?
Recovery isn’t quick. Even if the surgery works, your eye needs time to heal. If you had a gas bubble, you’ll need to keep your head in a specific position for days. No flying. No scuba diving. The gas expands at high altitude and can cause blindness. You’ll use eye drops for weeks-antibiotics and anti-inflammatories. You might feel grittiness, redness, or mild discomfort. That’s normal. But complications happen. About 25% of patients get higher eye pressure. About 5-15% have another detachment. And as mentioned, most people who had vitrectomy will need cataract surgery within two years. Follow-up visits are critical. Your doctor will check your retina with OCT and ultrasound every few weeks for months. Missing a follow-up could mean a missed recurrence.What’s New in Treatment?
Technology is improving. New 27-gauge vitrectomy systems (like the EVA Platform) use smaller incisions, less trauma, and faster healing. Intraoperative OCT lets surgeons see the retina in real time during surgery, improving precision. Researchers are testing bioengineered retinal patches and gene therapies for inherited conditions that cause detachment. These aren’t ready yet-but they’re coming. The biggest change? AI-assisted screening. In the next five years, AI tools may help detect early signs of retinal tears in routine eye scans, catching problems before they become emergencies.What to Do Right Now
If you’ve noticed any of the six symptoms:- Don’t wait. Don’t call your regular doctor. Go to an emergency eye clinic or hospital with an ophthalmology department.
- Bring your glasses or contacts. The doctor needs to know your prescription.
- Don’t drive yourself if your vision is blurry or you have a curtain over your eye. Get a ride.
- Write down when the symptoms started and how they’ve changed. This helps the doctor.
If you’re at high risk-nearsighted, had cataract surgery, or have lattice degeneration-get a dilated eye exam every year. Even if you feel fine. Retinal tears often happen without symptoms. And if caught early, a simple laser procedure can prevent a full detachment.
Retinal detachment isn’t something you can treat with eye drops or rest. It’s not a myth. It’s real. And it’s fast. Your vision doesn’t come back if you wait too long. Recognize the signs. Act fast. Save your sight.
Can retinal detachment fix itself?
No. A detached retina will not heal on its own. Without surgery, the photoreceptor cells in the retina begin to die within hours. Once they die, vision loss is permanent. Even if the symptoms seem to fade, the detachment hasn’t reversed-it may have stabilized temporarily, but the risk of total vision loss remains high. Immediate surgical repair is the only way to restore vision.
Is retinal detachment painful?
No, retinal detachment itself is not painful. There’s no ache, pressure, or redness. That’s why it’s so dangerous. People often ignore the warning signs because they don’t feel sick. The only symptoms are visual: floaters, flashes, shadows, or blurry vision. If you feel eye pain, it’s likely something else-like glaucoma or uveitis-but you should still get it checked immediately.
Can I fly after retinal detachment surgery?
No-not if you had a gas bubble injected into your eye. At high altitudes, the gas expands and can cause severe pressure buildup inside your eye, leading to pain, blindness, or permanent damage. You must avoid flying, driving to high elevations, or even going on a mountain hike until the gas is fully absorbed, which can take 2-8 weeks depending on the type of gas. Your surgeon will tell you exactly when it’s safe. Silicone oil doesn’t have this restriction, but it requires a second surgery to remove.
How long does recovery take after retinal detachment surgery?
Full recovery takes 2 to 6 months. Vision improves gradually. You may notice blurry or distorted vision for weeks. If you had a gas bubble, you’ll need to maintain a specific head position for 7-10 days. Most people return to light activities after 2-4 weeks, but heavy lifting, bending, or strenuous exercise should be avoided for at least 6 weeks. Your surgeon will guide you based on the type of surgery and your healing progress.
Will I need glasses after surgery?
You may need new glasses after surgery, especially if you had scleral buckling or vitrectomy. Scleral buckling can cause new nearsightedness, requiring stronger prescriptions. Vitrectomy often leads to cataracts within two years, which also changes your vision. Many patients end up needing reading glasses or bifocals after surgery, even if they didn’t before. Your eye doctor will check your prescription 4-6 weeks after surgery and update it as needed.
Can retinal detachment happen again?
Yes. About 5-15% of patients experience another detachment, even after successful surgery. The risk is higher if you have severe nearsightedness, a history of trauma, or developed scar tissue (proliferative vitreoretinopathy) after surgery. That’s why follow-up exams are critical. If you notice any new floaters, flashes, or shadows after surgery, contact your doctor immediately-even if it’s months later.
Jeffrey Frye
December 24, 2025 AT 09:48Aurora Daisy
December 25, 2025 AT 09:45Usha Sundar
December 27, 2025 AT 05:06claire davies
December 29, 2025 AT 01:08Wilton Holliday
December 29, 2025 AT 13:35Raja P
December 30, 2025 AT 01:40Joseph Manuel
December 30, 2025 AT 20:01Harsh Khandelwal
December 31, 2025 AT 05:45Andy Grace
January 1, 2026 AT 22:08Delilah Rose
January 3, 2026 AT 20:18Spencer Garcia
January 5, 2026 AT 13:30Abby Polhill
January 5, 2026 AT 15:05CHETAN MANDLECHA
January 5, 2026 AT 20:09Jillian Angus
January 6, 2026 AT 17:39Pankaj Chaudhary IPS
January 8, 2026 AT 01:21