You took a pill, and within an hour, your skin broke out in a rash. Your first thought? Drug allergy. But what if it wasn’t? What if it was just a side effect - something common, harmless, and totally expected? Mixing up these two things isn’t just confusing - it can put your health at risk.
What’s Really Happening in Your Body?
A drug allergy means your immune system thinks the medication is an invader. It’s like your body’s alarm system going off for no reason. When that happens, it releases chemicals like histamine, which cause symptoms: hives, swelling, trouble breathing, or even life-threatening anaphylaxis. This isn’t just discomfort - it’s a biological overreaction.
Side effects, on the other hand, are built into the drug’s design. They’re not about your immune system. They’re about how the drug works in your body. For example, antibiotics like amoxicillin can cause diarrhea because they kill off good bacteria in your gut. Statins can cause muscle aches because they interfere with cholesterol production in muscle cells. These aren’t surprises - they’re documented, predictable outcomes.
Here’s the kicker: only 5 to 10% of people who say they have a drug allergy actually do. The rest? They’re describing side effects. That’s a huge gap - and it’s causing real harm.
Timing Tells the Story
One of the clearest ways to tell the difference is when the reaction happens.
If you get hives, swelling of the lips, or sudden wheezing within minutes to an hour after taking a drug - especially penicillin, sulfa, or NSAIDs - that’s a red flag for a true allergy. These are IgE-mediated reactions. They’re fast. They’re serious. And they need immediate attention.
But if you start feeling nauseous, dizzy, or get a mild rash two or three days in - and it gets better as you keep taking the pill - that’s likely a side effect. Many side effects fade after your body adjusts. Diarrhea from metformin? Often gone after a week. Dry cough from ACE inhibitors? Happens in up to 20% of users, but doesn’t mean you’re allergic.
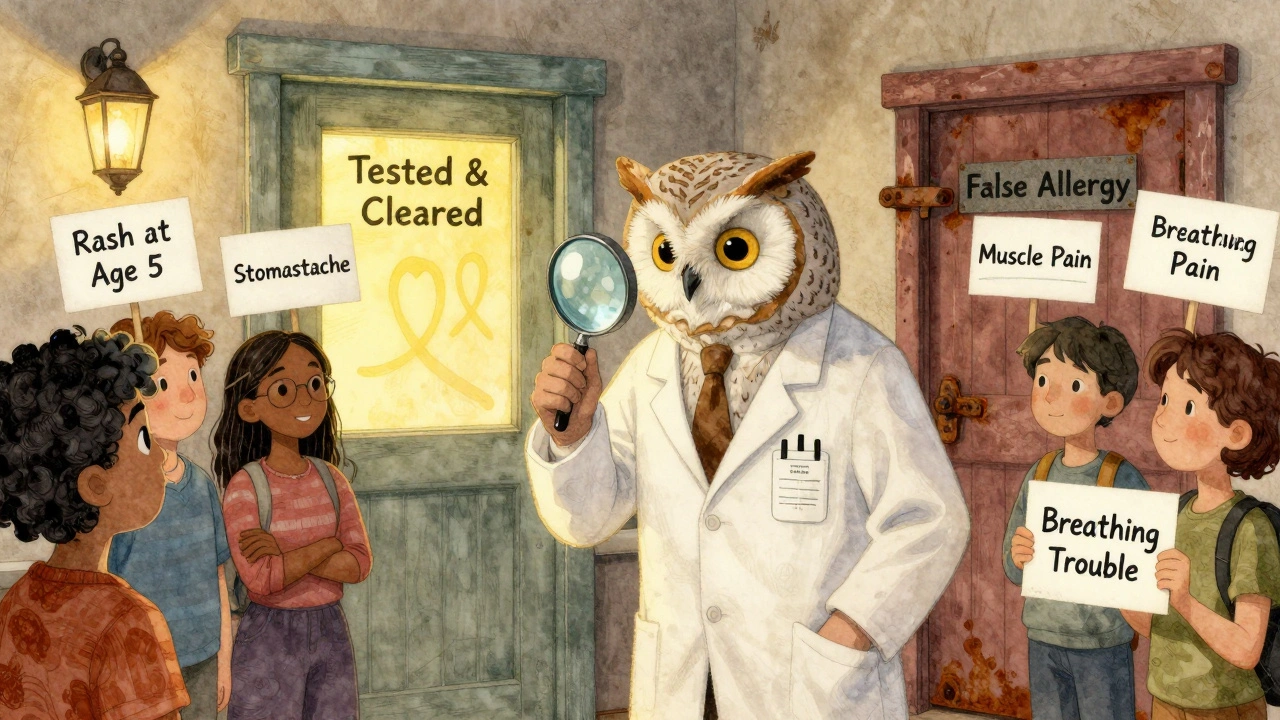
Delayed reactions are trickier. A rash that shows up two weeks after starting amoxicillin? It might look like an allergy, but in kids, it’s often caused by a virus they had at the same time. Studies show up to 90% of these cases are mislabeled as allergies. That’s why doctors don’t just take your word for it - they ask for details.
Common Drugs, Common Confusions
Some drugs are more likely to cause confusion than others.
- Penicillin: The most common drug allergy label. But 95% of people who think they’re allergic to penicillin can take it safely after testing. Many were told they were allergic because they got a rash as a child - often from a virus, not the drug.
- Sulfa antibiotics: People say they’re allergic because they got a rash or upset stomach. But true sulfa allergy is rare. Most reactions are side effects. Avoiding sulfa drugs unnecessarily means doctors use stronger, more expensive antibiotics - which fuels antibiotic resistance.
- NSAIDs like ibuprofen: Stomach upset? Common side effect. But if you get swelling or breathing trouble, that’s a true allergy - and you need to avoid all NSAIDs.
- Statins: Muscle pain is a known side effect. It’s not an allergy. Stopping them because you think you’re allergic can increase your risk of heart attack or stroke.
- Chemotherapy drugs: Nausea, fatigue, hair loss - these are expected side effects. They’re not allergies. Mistaking them for allergies can delay life-saving treatment.
The biggest danger? Being labeled allergic when you’re not. If you’re wrongly labeled as penicillin-allergic, you’re 69% more likely to get a broad-spectrum antibiotic like vancomycin. That increases your risk of getting a deadly C. diff infection by 2.5 times.

Why Mislabeling Costs Lives - and Money
This isn’t just about health. It’s about money too.
Patients with a mislabeled penicillin allergy cost the U.S. healthcare system over $1 billion a year. Why? Because they get more expensive, less effective drugs. Their hospital stays are longer. Their recovery is slower.
One study found that patients with a penicillin allergy label paid $1,025 more per hospital stay - not because they were sicker, but because their treatment options were limited.
And it’s not just antibiotics. If you’re labeled allergic to sulfa, you might miss out on the best treatment for a urinary tract infection. If you avoid statins because you think you’re allergic, you might end up in the ER with a heart attack.
Doctors are starting to catch on. Hospitals are hiring pharmacists to review allergy lists. Electronic health records now prompt providers to ask: “What exactly happened?” instead of just accepting “allergic.”
What You Can Do: Ask the Right Questions
If you think you have a drug allergy, don’t just accept the label. Dig deeper.
Ask yourself:
- What exactly happened? (Rash? Swelling? Nausea? Trouble breathing?)
- When did it start? (Within an hour? After a few days?)
- Did you need emergency treatment? (Epinephrine? Hospitalization?)
- Did it happen every time you took the drug?
- Was there another illness going on? (Like a virus or infection?)
If you’re unsure, talk to your doctor. Ask if you should see an allergist. Skin testing for penicillin is safe, quick, and 97% accurate. A supervised oral challenge - where you take a small dose under medical supervision - can confirm whether you’re truly allergic.
And if you’ve been told you’re allergic but never had a serious reaction? You might be able to get that label removed. Many people do. And it changes everything.
What to Do If You’re Really Allergic
Not everyone who says they’re allergic is wrong. Some people truly have life-threatening reactions.
If you’ve had anaphylaxis - low blood pressure, swelling of the throat, loss of consciousness - after a drug, you need to avoid it forever. Carry an epinephrine auto-injector. Wear a medical alert bracelet. Make sure your family and doctors know.
For delayed reactions like DRESS syndrome (a rare but deadly skin reaction with fever and organ involvement), you need to avoid not just the drug, but similar ones. For example, if you had DRESS from carbamazepine, you can’t take other anticonvulsants like phenytoin without genetic testing.
These are real allergies. And they need real caution.
The Bottom Line: Know the Difference
Drug allergies are rare. Side effects are common. But we treat them the same way - and that’s dangerous.
Getting the right diagnosis isn’t about being right. It’s about getting the right treatment. It’s about avoiding unnecessary risks. It’s about saving money - and possibly your life.
If you’ve ever been told you’re allergic to a drug, take a moment. Ask yourself: Was it really an allergy? Or just a side effect? And if you’re not sure - get it checked. You might be surprised at what you find.
How do I know if my reaction was a drug allergy or just a side effect?
Look at the timing and symptoms. If you had hives, swelling, trouble breathing, or low blood pressure within minutes to an hour after taking the drug, it’s likely a true allergy. If you had nausea, diarrhea, dizziness, or a mild rash that started days later and improved over time, it’s probably a side effect. True allergies involve your immune system; side effects are direct effects of the drug’s chemistry.
Can I outgrow a drug allergy?
Yes - especially with penicillin. About 80% of people who had a penicillin allergy as a child lose it within 10 years. That’s why it’s important to get tested, even if you were labeled allergic decades ago. Many people who think they’re allergic can safely take the drug again after proper evaluation.
Is it safe to try a drug again if I had a mild reaction before?
Never try a drug again on your own after any reaction. But under medical supervision - with a doctor or allergist - a controlled challenge can be very safe. For low-risk reactions (like a mild rash), oral challenges start with 1-10% of the full dose and are closely monitored. Over 95% of low-risk patients complete the test without issue.
Why do so many people think they’re allergic to penicillin?
Most people are labeled allergic after a childhood rash - often from a virus like mononucleosis, not the drug. Back then, doctors didn’t have good tests, so they just said “allergy.” Now we know better. Up to 95% of people with that label can safely take penicillin. But without testing, the label sticks - and limits treatment options.
What should I do if I’m told I have a drug allergy?
Don’t just accept it. Write down exactly what happened - symptoms, timing, treatment needed. Then ask your doctor: “Could this have been a side effect?” If it was mild or unclear, ask for a referral to an allergist. Testing can remove a false label and open up better, safer treatment options.
Can a drug allergy be diagnosed with a blood test?
For most drugs, no. Blood tests for IgE antibodies exist only for a few drugs, like penicillin, and even those aren’t perfect. Skin testing is still the gold standard. For delayed reactions like DRESS, doctors look for signs like high eosinophil counts and liver enzyme changes - not blood tests for allergy. Diagnosis is based on timing, symptoms, and ruling out other causes.

Donna Hammond
December 13, 2025 AT 07:09This is such an important post. I used to think I was allergic to penicillin because I got a rash as a kid - turns out it was mono. Got tested last year and now I can take it safely. My doctor said I saved myself years of unnecessary antibiotics. Thank you for clarifying the difference.
So many people don’t realize how much this impacts their care. If you’ve been told you’re allergic, don’t just accept it. Ask for a referral. It’s not scary - it’s life-changing.
Richard Ayres
December 14, 2025 AT 13:06While the distinction between allergic reactions and side effects is clinically sound, it is imperative that patients not self-diagnose based on internet content. The nuances of immune-mediated responses require professional evaluation. That said, the data presented here is robust and aligns with current guidelines from the American Academy of Allergy, Asthma & Immunology.
Healthcare systems must prioritize allergy de-labeling programs. The economic and clinical burden of misclassification is substantial and under-addressed.
Sheldon Bird
December 14, 2025 AT 19:36Yessss!! This is exactly what we need more of 💪
I had the same thing - thought I was allergic to ibuprofen because my stomach hurt. Turns out I just took it on an empty stomach. Now I take it with food and no issues. So many people are unnecessarily avoiding meds because they don’t know the difference. Keep spreading this info!! 🙌
Karen Mccullouch
December 16, 2025 AT 11:27Of course they downplay allergies. Big Pharma doesn’t want you to know how many drugs are toxic. They profit off people being labeled ‘allergic’ so they can push more expensive, dangerous alternatives. They don’t care if you get C. diff - they get paid either way.
They’ll tell you it’s ‘just a side effect’ while hiding the real danger. Trust your body. If it reacts, it’s not ‘just’ anything. It’s a warning.
And why are they suddenly testing penicillin? Because they want you to take it again so they can sell you more pills. Wake up.
Ronan Lansbury
December 18, 2025 AT 01:23How convenient that the medical establishment suddenly has a ‘solution’ to the ‘mislabeling’ problem - right after patent expiries on penicillin analogs. The entire allergy narrative is a controlled narrative designed to funnel patients toward newer, proprietary antibiotics with higher profit margins.
Have you considered that the 95% ‘false allergy’ statistic is manufactured? Who funded that study? Who owns the skin test kits?
I’m not saying it’s wrong - I’m saying it’s too tidy. Too convenient. Too… corporate.
Jennifer Taylor
December 19, 2025 AT 06:31OMG I CRIED reading this 😭
I’ve been labeled allergic to sulfa since I was 12 because I got a rash after a UTI - turns out I had a yeast infection AND the antibiotic didn’t work, so they just said ‘allergy.’ I’ve been avoiding Bactrim for 20 years. I just got tested last month and I’m NOT allergic. I’m SO mad I wasted all those years with clindamycin and cipro when I could’ve had the BEST drug for my bladder.
Also my mom thinks I’m crazy now because I told her I’m not allergic anymore. She said ‘But you were always allergic!’ Like my body’s memory is a family legend now 😭
ANYONE ELSE FEEL THIS??
PS I’m telling my entire family to get tested. This is life-changing.
Shelby Ume
December 20, 2025 AT 15:57Thank you for writing this with such clarity. As someone who works in primary care, I see this every single day.
Patients come in saying, ‘I’m allergic to statins,’ and when we ask what happened, they say, ‘My legs hurt.’ That’s not an allergy - that’s a side effect, and it often goes away with dose adjustment or switching statins.
But because they’ve been told ‘allergy,’ they won’t take anything. And then they come back six months later with chest pain.
We need more of this education - not just for patients, but for doctors too. Not every reaction is an allergy. Not every rash is anaphylaxis.
Please share this with your loved ones. It could save their life.
Jade Hovet
December 22, 2025 AT 03:15so i got this rash after taking amoxicillin when i was 7 and now im 34 and i still avoid all antibiotics 😅
but like... i just got tested last month and turns out i was never allergic?? i had a virus and the rash was just a thing that happens sometimes with viruses and amoxicillin??
so now im like... why did i avoid penicillin for 27 years??
my doctor said i could’ve taken it for my ear infection last year and saved myself from 2 weeks of cipro 😭
also i cried. this is wild.
if you think you're allergic - get tested. it’s like 20 minutes. you’re not broken. you’re just misinformed. 💙
nithin Kuntumadugu
December 23, 2025 AT 00:22lol american medical system again. first they give you the drug, then they tell you you're allergic so you can't use the real medicine, then they sell you the expensive one. it's a scam. i saw this in india too - doctors label everything 'allergy' so they can prescribe branded drugs. no one cares if you live or die, only if they get paid.
penicillin? 10 cents. vancomycin? $500. who wins? not you.
they don't want you to know you're not allergic. they want you to keep buying the expensive stuff.
and now they want you to pay for a test to prove it? lmao. classic.
John Fred
December 24, 2025 AT 17:56From a clinical pharmacology standpoint, this is a textbook example of therapeutic misclassification. The IgE-mediated hypersensitivity paradigm is often conflated with non-immunologic adverse drug reactions - particularly with beta-lactams and NSAIDs.
What’s critical is the differential timing: immediate vs. delayed hypersensitivity. The 5–10% true allergy rate is well-documented in JAMA and NEJM meta-analyses.
Also, the economic burden metric - $1B/year in the US - is conservative. Add in downstream complications like C. diff and MRSA, and it’s closer to $3.5B. This isn’t just clinical - it’s a systems failure.
Bottom line: De-labeling = better outcomes + lower costs. We need mandatory allergy reviews in EHRs. #Pharmacoepidemiology
sharon soila
December 25, 2025 AT 23:02Every person deserves to know the truth about their body.
If you’ve been told you’re allergic to a drug, please don’t live in fear of it. You didn’t fail. You were misinformed.
It’s not your fault. It’s the system’s.
But now you know. And knowledge is power.
Take a deep breath. Call your doctor. Ask for a referral. It’s not complicated. It’s not scary. It’s just… right.
You’re not broken. You’re just waiting for the right information.
And you deserve better.
nina nakamura
December 27, 2025 AT 20:40So you’re telling me people are too dumb to tell the difference between a rash and anaphylaxis? That’s why we have 10x the cost of care. This isn’t a medical problem - it’s a human one. People believe everything they hear. They don’t read. They don’t think. They just scream ‘allergy’ and demand to be heard. Now we’re stuck with bloated healthcare bills because no one wants to be wrong.
Stop being lazy. Learn the difference. Or stop complaining about costs.
Cole Newman
December 28, 2025 AT 11:38Bro I had the exact same thing. Told I was allergic to penicillin at age 5 after a rash. 25 years later I’m like… wait, I took it for my sinus infection last year and I was fine? Turns out my mom just told the doctor ‘she broke out’ and they wrote ‘allergy’ without asking anything.
I got tested. Zero reaction. I’m not allergic. I’m just… a victim of bad documentation.
And now my sister is scared to take it because ‘mom said you’re allergic.’
Why do we still do this? Why is it so hard to fix?
Emily Haworth
December 28, 2025 AT 22:16they’re hiding something. why now? why are they suddenly testing penicillin allergies? why not 20 years ago? why not when we were kids?
what if the real reason is that they want to push new antibiotics that aren’t generic yet? what if they need people to believe they’re allergic so they can sell the expensive ones?
and what if the ‘95% false allergy’ stat is just a marketing tool?
i don’t trust them anymore. i’ve seen too much.
if you’re allergic, you’re allergic. don’t let them convince you otherwise. your body knows better than any test.
Donna Hammond
December 29, 2025 AT 09:51Just saw your comment about your sister being scared - that’s exactly why this matters. I had the same thing. My mom still says I’m allergic even though I’ve taken penicillin three times since my test. She says, ‘But what if it’s different this time?’
It’s not fear of the drug. It’s fear of being wrong.
And that’s the real problem.
We’re not just mislabeling drugs - we’re mislabeling trust. In our bodies. In our doctors. In science.
So I keep telling my story. Because if one person reads this and gets tested… it’s worth it.